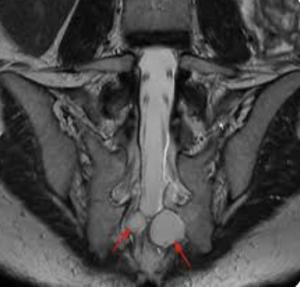
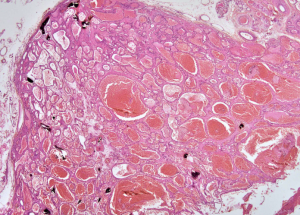
In a single-center retrospective cohort study (n=41) Jin Zhu et al. from the Beijing Jishuitan Hospital, published in Neurosurgical Review to assess clinical predictors of symptom improvement following reinforced radiculoplasty in patients with symptomatic sacral Tarlov cysts (TCs). Reinforced radiculoplasty significantly improves pain and numbness in sacral TC patients. Greater likelihood of pain-free status is associated with older age and lower preoperative VAS scores. No variables significantly predicted numbness relief 1).
Critical Review:
The study targets an underexplored treatment avenue—reinforced radiculoplasty—for symptomatic Tarlov cysts, an entity often managed conservatively due to unclear pathophysiology and outcome data. The authors utilize a small retrospective sample, limiting statistical power and generalizability. While binary logistic regression is appropriately applied, the absence of a control group and the reliance on telephone follow-ups raise concerns regarding recall bias and subjective assessment of outcomes. Furthermore, the study fails to delineate surgical technique variability or operator-dependence, critical factors in neurosurgical outcome studies. The lack of correlation with imaging changes and omission of bowel/bladder symptom stratification are notable limitations.