1. Predictable Yet Pointless
The authors claim novelty by describing a rare anatomical presentation of EA. However, this degenerates into a predictable narrative with no new pathophysiological insights, no hypothesis generated, and no clinical paradigm challenged. It is the kind of “rare case” that proliferates in low-barrier journals precisely *because* it demands no intellectual risk.
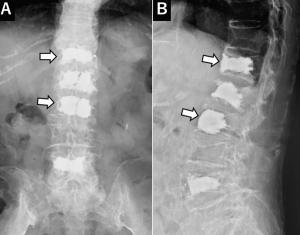
2. Zero Diagnostic Value
The authors bypass the opportunity to deepen our understanding of the radiological-morphological signature of EA in the spine. No comparative imaging, no differential diagnostic flowchart, no histopathological discussion beyond standard CD31/CD34 immunostaining. If this case had been published in 1995, it would be equally uninformative.
3. Therapeutic Confusion Disguised as Aggressiveness
Two major spine surgeries (posterior decompression + anterior corpectomy) followed by immediate radiotherapy in a moribund patient demonstrate therapeutic overreach without oncological strategy. There is no discussion on multidisciplinary planning, palliative thresholds, or whether delaying surgery or avoiding the second procedure might have prevented ARDS. The reader is left with the impression of a surgical reflex, not an evidence-based decision.
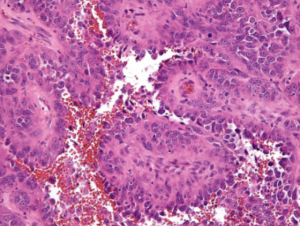
4. No Discussion of Differential Diagnosis or Biomarkers
In a tumor type notorious for being misdiagnosed as metastasis, chordoma, or sarcoma NOS, the absence of a differential diagnostic framework or advanced markers (ERG, FLI1, HHV-8, etc.) is alarming. Histological laziness cloaked in “rare disease” rhetoric.
5. Outcome Reporting: Conveniently Truncated
The patient dies 3 weeks after surgery, yet the discussion fails to draw any causal or cautionary link between the interventions and the fatal ARDS. No autopsy data, no postmortem imaging, no pulmonary workup. This omission sterilizes the clinical narrative, reducing it to anecdote.
6. Ethically Murky
The case implicitly raises an ethical dilemma—should maximal surgery be performed in aggressive, terminal tumors without demonstrated systemic control? Yet the authors shy away from even mentioning this, let alone framing it for academic discussion.
7. Journal Choice Reflects the Paper’s Weakness
Published in a journal known for minimal peer review stringency, the article offers no citations of recent molecular or targeted therapy advances, no engagement with broader oncological guidelines, and no rationale for the treatment decisions beyond procedural listing.
This case report is an example of procedural reporting devoid of scientific merit, clinical reflection, or ethical introspection. It contributes nothing to the understanding of EA, its diagnosis, biology, or management—beyond reiterating its rarity. In its current form, it is neither hypothesis-generating nor practice-changing, and serves as a cautionary tale on how not to write a case report.