Middle meningeal artery embolization for chronic subdural hematoma
Middle meningeal artery embolization is effective for Chronic subdural hematoma recurrence, and is considered an effective therapeutic method to stop hematoma enlargement and promote resolution 1) 2) 3) 4) 5) 6).
A pilot study indicated that perioperative middle meningeal artery (MMA) embolization could be offered as the least invasive and most effectual means of treatment for resistant patients of CSDHs with 1 or more recurrences 7).
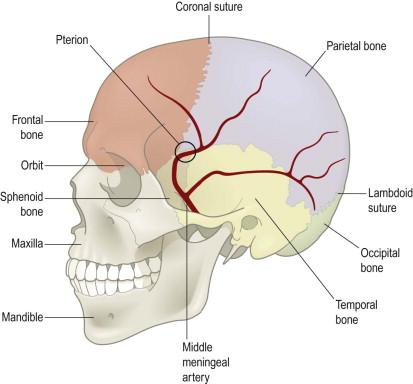
Chihara et al. have treated three cases of CSDH with MMA embolization to date, but there was a postoperative recurrence in one patient, which required a craniotomy for hematoma removal and capsulectomy. MMA embolization blocks the blood supply from the dura to the hematoma outer membrane in order to prevent recurrences of refractory CSDH. Histopathologic examination of the outer membrane of the hematoma excised during craniotomy showed foreign-body giant cells and neovascular proliferation associated with embolization. Because part of the hematoma was organized in this case, the CSDH did not resolve when the MMA was occluded, and the development of new collateral pathways in the hematoma outer membrane probably contributed to the recurrence. Therefore, in CSDH with some organized hematoma, MMA embolization may not be effective. Magnetic resonance imaging (MRI) should be performed in these patients before embolization 8).
Perioperative prophylactic Middle meningeal artery embolization in the setting of surgical evacuation, via either craniotomy or subdural evacuating port system (SEPS), may help to lower the recurrence rate of cSDH 9).
It can be used safely and effectively as an alternative or adjunctive minimally invasive chronic subdural hematoma treatment in elderly and advanced elderly patients 10).
It has been proposed as a curative treatment for chronic subdural hematoma (cSDH), but evidence for the indication and timing is not definitive.
Complications
Trials
Systematic Reviews
Narrative reviews
The incidence and prevalence is expected to grow due to aging of the population and the increase in anticoagulation and anti-aggregation prescription drugs. Traditionally, it was accepted that the bleeding originates from bridging veins that drain the brain towards the dural sinuses. However, recent findings exposed an additional underlying mechanism. Trauma leads to separation of the dural border cell layer which induces an inflammatory process that starts positive feedback of leaky blood vessels formation (angidysgensis), which causes blood product leakage that further increases the inflammation. For many years, the disease has been treated conservatively in cases of mild clinical and imaging features, or by surgical evacuation of the hematoma in more severe cases. The literature shows a consistent high recurrence rate of around 30% following a surgical removal of the blood. The newly discovered mechanism inspired the development of a novel treatment method for this entity. Endovascular embolization of the middle meningeal artery (MMA). This method has an excellent efficacy and safety profile, and it can be performed alone or in combination with surgical evacuation. A review of Milikovsky et al. presents the epidemiology and mechanisms underlying CSDH, in addition to possible treatment methods, and eventually discuss MMA embolization to increase the awareness of the medical community in Israel to this new approach 11).
Case series
Case reports
A 70-year-old male with ischemic heart disease, diabetes mellitus, and hypertension who presented with worsening headaches for the past three days, associated with gait imbalance and dizziness. The patient was vitally stable on examination with a Glasgow Coma Scale/Score (GCS) of 15/15; his pupils were reactive bilaterally; and his neurological examination was unremarkable. Non-contrast computed tomography (CT) of the head yielded acute and Chronic Subdural Hematoma. The patient was initially managed by middle meningeal artery embolization, but one day later he developed a stroke. Hence, thrombectomy and burr hole craniotomy were performed to manage the stroke and evacuate the chronic subdural hematoma (CSDH). This paper presents this case as uncommon acute on chronic SDH presented with headache and vertigo, treated with embolization and with complications of stroke and pulmonary embolism 12).
A case of a 74-year-old male on aspirin with a history of recurrent symptomatic chronic right-sided subdural hematoma treated successfully with a SEPS and right middle meningeal artery embolization with poly vinyl alcohol (PVA) microparticles. The patient initially presented to the emergency department with headaches, difficulty walking, and left sided hemiparesis. CT Head showed a large chronic right-sided subdural hematoma measuring 2.7 cm thick with 1 cm of leftward shift. Patient underwent placement of a right-sided SEPS and the subdural hematoma decreased in size to 1.0 cm with 2 mm of leftward shift. The patient had resolution of headaches and neurological symptoms and was discharged home. Three months later, the patient returned to the emergency department with headache and left hand numbness. CT Head showed an acute on chronic right-sided subdural hematoma measuring 1.4 cm with 3 mm of leftward shift. Patient underwent right-sided SEPS placement. Repeat CT Head showed reduction in the subdural hematoma to 1.2 cm. The SEPS was removed and the patient had resolution of neurological symptoms. The patient then had a diagnostic cerebral angiogram with PVA microparticle embolization of the right middle meningeal artery. A SEPS was placed at the time of the angiogram to further reduce the size of the subdural hematoma.
Repeat CT Head after SEPS and middle meningeal artery embolization showed decrease in size of the subdural hematoma. Follow-up CT Head showed stability of the subdural hematoma and patient had no further neurological symptoms. Patient was discharged home.
Middle meningeal artery embolization is a useful endovascular technique for reducing the arterial supply to the membranes in chronic subdural hematomas. Middle meningeal artery embolization can reduce the recurrence rate of subdural hematomas 13).
In 1994 a rare case of chronic subdural hematoma associated with a middle meningeal arteriovenous fistula was treated by a combination of embolization and burr hole drainage. This clinical situation might be missed in this era of computed tomography, when cerebral angiography is seldom indicated for the diagnosis of neuro-traumatic diseases. We should bear in mind the possibility of this clinical situation of a chronic subdural hematoma associated with a linear skull fracture crossing the middle meningeal groove in order to avoid possible hemorrhagic complications during surgery for chronic subdural hematoma 14).