In a retrospective cohort Ishida *et al.* from the University hospitals—centres in Tokyo, (e.g., Tokyo Metropolitan Geriatric Center) published in the *Journal of Magnetic Resonance Imaging* to compare interstitial fluid volume fraction (Fint) and diffusivity (Dint), derived via spectral diffusion analysis, between idiopathic normal pressure hydrocephalus (iNPH) patients and healthy controls (HCs). In iNPH patients, spectral diffusion analysis revealed increased Fint and Dint in periventricular hyperintensity (PVH) regions of the centrum semiovale (CSO) and frontal white matter (FWM), while regions outside PVH did not differ from HCs 1).
Critical Review
* Strengths:
-
Utilizes advanced spectral diffusion with non‑negative least squares to separate Interstitial Fluid Dynamics an innovative approach.
-
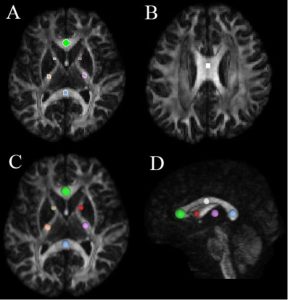
Well‑defined region‑based ROI analysis including CSO, FWM, lenticular nucleus (LN).
-
Robust statistical treatment via Kruskal–Wallis with Dunn’s test; Spearman’s for correlations.
* Limitations & Concerns:
-
Retrospective design: susceptible to selection bias, especially with mismatched age demographics (mean HC age 47.5 vs iNPH 76.9 years).
-
Age confounders: ISF measures increase with age; healthy ≥60 group is younger on average and unevenly represented, raising questions about matching.
-
Lack of clinical correlation: imaging findings are intriguing but lack direct linkage to symptom severity or treatment outcome.
-
No intervention arm: absence of longitudinal or shunt response data means limited clinical applicability.
Final Verdict
Score: 5.5 / 10 Spectral diffusion yields promising imaging biomarkers for PVH-affected regions in iNPH, but substantial limitations (age confounders, lack of clinical linkage, retrospective nature) undermine its current translational value.
Takeaway for Practicing Neurosurgeon
Spectral diffusion analysis identifies increased interstitial fluid volume and diffusivity in periventricular hyperintensity regions of elderly iNPH patients. However, due to age confounding and absence of correlation with clinical outcomes or shunt responsiveness, these metrics remain research curiosities rather than clinical tools. Prospective studies—ideally age-matched and linked to gait/cognitive improvement post-shunt—are needed before integrating into practice.
Bottom Line
Spectral diffusion draws attention to altered ISF dynamics in iNPH, yet further longitudinal, clinically-correlated validation is required before adoption.
Clinical Implications:
-
SDA-derived metrics may aid in:
-
Early, pathophysiology-based diagnosis of iNPH
-
Differentiation from other causes of ventriculomegaly (e.g., atrophy)
-
Predicting shunt responsiveness
-
-
Provides insight into the glymphatic dysfunction hypothesis of iNPH
Advantages:
-
Non-invasive, quantitative
-
Detects subtle extracellular fluid alterations before gross morphological changes
-
Applicable in clinical MRI with multi-b-value acquisition
Limitations:
-
Requires advanced MRI acquisition and post-processing
-
Interpretation depends on validation of model assumptions
-
Not yet widely available in routine clinical practice