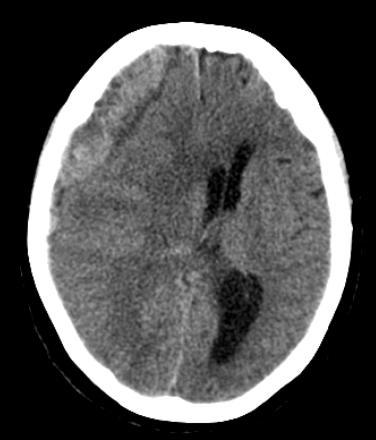
Subacute traumatic subdural hematoma
Subacute subdural hematomas are defined arbitrarily as those that present between 4 and 21 days after injury.
Traumatic subacute subdural hematoma is a condition in which the major symptoms affecting prognosis most appear in the subacute stage after head trauma, while traumatic acute subdural hematoma is treated conservatively when the symptoms are mild. The cause of the major symptoms occurring in the subacute stage is mostly expansion of the subdural hematoma volume.
Traumatic subacute subdural hematomas can usually be evacuated via craniotomy under general anesthesia.
Case reports
a case of malignant right-sided MCA/PCA infarction in a 62-year-old man who presented with progressive headache following a cycling incident leading to a head injury. Initial CT head demonstrated a small right ASDH. He had no neurological deficit, headache settled on analgesia, and there was no expansion of the SDH on the repeat CT; therefore, he was managed conservatively. He was admitted 6-days later with worsening headaches and hyponatremia. Repeat CT revealed an increase in size of the hematoma and mass effect leading to a mini-craniotomy and evacuation of hematoma. He developed left-sided hemiplegia, slurred speech and hyponatremia, and CT head demonstrated a right-sided MCA/PCA infarction with significant mass effect. He underwent emergent DC and subsequent cranioplasty and ultimately recovered to mRS of 2.
Conclusion: SDH are frequent neurosurgical entities. Malignant MCA/PCA strokes following mini-craniotomies are rare but need to be considered especially during the consent process 1)
2015
Ueba et al. report a traumatic subacute subdural hematoma in an elderly patient that was evacuated by endoscopic burr hole surgery using a curettage and suction technique under local anesthesia. This minimally invasive neurosurgery may lower the morbidity rate in elderly or sick patients with serious cardiac and/or pulmonary lesions in whom the inherent risks of general anesthesia are high.
An 88-year-old man was referred to our institution with left hemiparesis 6 days after sustaining a head injury. He was on antiplatelet drugs for severe coronary and peripheral artery disease and underwent hemodialysis three times a week.
Endoscopic burr hole surgery using a curettage and suction technique resulted in the complete evacuation of his subacute subdural hematoma and complete hemostasis, and he recovered completely.
Endoscopic burr hole surgery using a curettage and suction technique is a minimally invasive treatment to address subacute subdural hematomas. This method may be particularly useful in older patients in whom general anesthesia poses additional risks 2).
1998
Nishio et al report a case of traumatic subacute subdural hematoma in which the cause of the major symptoms was cerebral hemispheric edema instead of expansion of the subdural hematoma volume.
Only one similar case to the present case has been previously reported. A 44-year-old female fell from the stairs on July 21, 1995 and was suffering from headache. On July 23, she was admitted to the hospital because of generalized convulsion. On admission, she was drowsy but showed no convulsion. Head CT showed an acute subdural hematoma on the right side with a slight midline shift and no other abnormalities. She was treated conservatively because of the mildness of the symptoms and two days later became alert with no symptoms. Thereafter she only complained of occasional headache which was controlled with medicine. On August 3, she suddenly fell into coma. Head CT showed severe cerebral hemispheric edema on the right side without change of the subdural hematoma size. Emergency cerebral angiography showed no definitive abnormalities such as occlusion of the arteries or of the venous sinuses. Craniotomy associated with external decompression was performed. The hematoma was composed of red-brown jelly accompanied with some liquid component and had a thin black-brown outer membrane. While removing the hematoma, bleeding from a vein on the cerebral surface around the sylvian fissure was observed and this location was suspected to be the sources of the bleeding point. Postoperatively, she received steroid and barbiturate therapy associated with moderate hypothermia under hyperventilation. She tolerated this treatment well and left the hospital, on September 26, 1995 with only diplopia during downward gaze. Although the mechanisms of the cerebral hemispheric edema occurring in the subacute stage was unclear, a failure in the cerebral venous circulation arising from compression to the bridging veins, which may be hypoplastic, by the subdural hematoma was suspected to have been the cause 3).