Stereoelectroencephalography
Indications
Stereoelectroencephalography (sEEG) is a diagnostic procedure for a patient with refractory focal epilepsy that is performed to localize and define the epileptogenic zone. In contrast to grid electrodes, sEEG electrodes are implanted using minimal invasive operation techniques without large craniotomies. Stereoelectroencephalography is one of the intraoperative EEG techniques currently used in the presurgical work-up, and it is well-distinguished from other invasive techniques, such as subdural grids and strips.
Stereoelectroencephalography can be safely, accurately, and effectively utilized in children under age 2 with good postoperative outcomes using standard SEEG equipment. With minimal modification, this procedure is feasible in those with immature skulls and guides the epilepsy team's decision-making for early and optimal epilepsy surgery through effective localization of seizure onset zones 1).
History
Stereoelectroencephalography (SEEG) was originally developed by Jean Talairach and Bancaud.
Many SEEG depth electrode implantation techniques involve the use of extensive technological equipment and shaving of the patient's entire head before electrode implantation 2).
Electrocortical stimulation mapping (ESM) is often performed in patients undergoing stereoelectroencephalography (SEEG) prior to epilepsy surgery, with the goal of identifying functional cortex and preserving it postoperatively. ESM may also evoke a patient's typical seizure semiology. The purpose of a study of Bank et al. was to determine whether the sites at which typical auras are evoked during ESM are associated with other known clinical and electrophysiologic biomarkers of the epileptogenic zone: the seizure onset zone (SOZ), the early spread zone (ES), and high-frequency oscillations (HFOs). They found that the sites at which auras were provoked were not consistently associated with known biomarkers (p = 0.09). They conclude that evoked auras during ESM may reflect electrical spread rather than true epileptogenicity, and that a larger study is needed to assess their potential value as independent epileptic biomarkers 3).
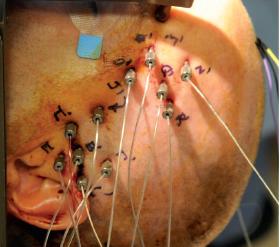
Stereoelectroencephalography electrode implantation
Stereoelectroencephalography guided radiofrequency thermocoagulation
Meta-analysis
Resective epilepsy surgery based on an invasive EEG-monitors performed with subdural grids (SDG) or depth electrodes (stereo-electroencephalography, SEEG) is considered to be the best option towards achieving seizure-free state in drug-resistant epilepsy. The authors present a meta-analysis, due to the lack of such a study focusing on surgical outcomes originating from SDG- or SEEG-monitors.
English-language studies published until May 2018, highlighting surgical outcomes were reviewed. Outcome measures including total number of SDG- or SEEG-monitors and resective surgeries; consecutively followed surgical cases; surgical outcomes classified by Engel in overall, temporal/extratemporal and lesional/nonlesional subgroups were analyzed.
19 articles containing 1025 SDG-interventions and 16 publications comprising 974 SEEG-monitors were researched. The rate of resective surgery deriving from SDG-monitoring hovered at 88.8% (95%CI:83.3-92.6%) (I2 = 77.0%;p < 0.001); in SEEG-group, 79.0% (95%CI:70.4-85.7%) (I2 = 72.5%;p < 0.001) was measured. After SDG-interventions, percentage of post-resective follow-up escalated to 96.0% (95%CI:92.0-98.1%) (I2 = 49.1%;p = 0.010), and in SEEG-group, it reached 94.9% (95%CI:89.3-97.6%) (I2 = 80.2%;p < 0.001). In SDG-group, ratio of seizure-free outcomes reached 55.9% (95%CI:50.9-60.8%) (I2 = 54.47%;p = 0.002). Using SEEG-monitor, seizure-freedom occurred in 64.7% (95%CI:59.2-69.8%) (I2 = 11.9%;p = 0.32). Assessing lesional cases, likelihood of Engel I outcome was found in 57.3% (95%CI:48.7%-65.6%) (I2 = 69.9%;p < 0.001), using SDG; while in SEEG-group, it was 71.6% (95%CI:61.6%-79.9%) (I2 = 24.5%;p = 0.225). In temporal subgroup, ratio of seizure-freedom was found to be 56.7% (95%CI:51.5%-61.9%) (I2 = 3.2%;p = 0.412) in SDG-group; whereas, SEEG-group reached 73.9% (95%CI:64.4%-81.6%); (I2 = 0.00%;p = 0.45). Significant differences between seizure-free outcomes were found in overall (p = 0.02), lesional (p = 0.031), and also, temporal (p = 0.002) comparisons.
SEEG-interventions were associated, at least, non-inferiorly, with seizure-freedom compared with SDG-monitors in temporal, lesional and overall subgroups 4).