Sonothrombolysis
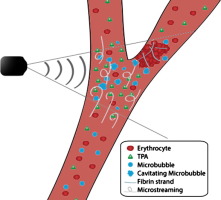 Ultrasound has been extensively investigated to promote clot lysis for the treatment of stroke, myocardial infarction, and acute peripheral arterial occlusions, with or without the use of tPA or contrast agents. In the age of modern minimally invasive techniques, magnetic resonance imaging-guided high intensity focused ultrasound is a new emerging modality that seems to promise therapeutic utilities for both ischemic and hemorrhagic stroke. High-intensity focused ultrasound causes thermal heating as the tissue absorbs the mechanical energy transmitted by the ultrasonic waves leading to tissue denaturation and coagulation. Several in-vitro and in-vivo studies have demonstrated the viability of this technology for sonothrombolysis in both types of stroke and have warranted clinical trials. Apart from safety and efficacy, initiation of trials would further enable answers regarding its practical application in a clinical setup. Though this technology has been under study for treatment of various brain diseases for some decades now, relatively very few neurologists and even neurosurgeons seem to be acquainted with it
1).
Ultrasound has been extensively investigated to promote clot lysis for the treatment of stroke, myocardial infarction, and acute peripheral arterial occlusions, with or without the use of tPA or contrast agents. In the age of modern minimally invasive techniques, magnetic resonance imaging-guided high intensity focused ultrasound is a new emerging modality that seems to promise therapeutic utilities for both ischemic and hemorrhagic stroke. High-intensity focused ultrasound causes thermal heating as the tissue absorbs the mechanical energy transmitted by the ultrasonic waves leading to tissue denaturation and coagulation. Several in-vitro and in-vivo studies have demonstrated the viability of this technology for sonothrombolysis in both types of stroke and have warranted clinical trials. Apart from safety and efficacy, initiation of trials would further enable answers regarding its practical application in a clinical setup. Though this technology has been under study for treatment of various brain diseases for some decades now, relatively very few neurologists and even neurosurgeons seem to be acquainted with it
1).
Recent studies have shown that inconsistent results of safety and efficacy between sonothrombolysis vs. non-sonothombolysis in acute ischemic stroke (AIS).
Chen et al., implemented a meta-analysis to explore the value of sonothrombolysis in AIS treatment. The MEDLINE, EMBASE, and Cochrane Library databases were searched for randomized controlled trials (RCTs) which had evaluated sonothrombolysis or ultrasound thrombolysis in AIS. One hundred five studies were retrieved and analyzed, among them, 7 RCTs were included in the current meta-analysis. In comparison with the non-sonothombolysis, sonothrombolysis significantly improved complete recanalization (RR 2.16, 95% CI 1.51 to 3.08, P < 0.001), complete or partial recanalization (RR 1.90, 95% CI 1.26 to 2.88, P = 0.002), there is also a tendency to improvement of ≥ 4 points in NIHSS score (RR 1.43, 95% CI 0.99 to 2.07, P = 0.057). However, sonothrombolysis and non-sonothrombolysis had insignificant differences in neurological recovery and adverse events. In subgroup analysis, they found that “With t-PA”, “NIHSS > 15”, “Treatment time ≤ 150min”, and “Age ≤ 65 years” are potential favorable factors for efficacy outcomes of sonothombolysis. Sonothrombolysis can significantly increase the rate of recanalization in patients with AIS compared with non-sonothrombolysis, but there is no significant effect on improving neurological functional recovery and avoiding complications 2).
In a study the sonothrombolytic efficacy of a new nanoscaled ultrasound contrast agent (NUSCA) was investigated. This new contrast agent has a size of less than 100 nm and should thus be able to penetrate the thrombus and achieve a thrombolysis from inside out. In this study human whole blood clots were exposed to US, US and NUSCA, US and recombinant tissue plasminogen activator (rt-Pa) or urokinase (UK), or a combination of US, NUSCA and thrombolytic drug in a closed-loop flow model. They sonicated with diagnostic US at a frequency of 2.85 MHz for 30 min. Clot mass loss of 50.6 ± 6.0% for the combination of US, NUSCA and rt-PA was found. Using UK as thrombolytic drug 57.7 ± 9.0% clot mass loss could be seen. Thus the weight loss exceeded the conventional values of up to 30%. Scanning electron microscopy (SEM) images revealed changes of the fibrin network on the thrombus surface. The NUSCA was able to loosen the network and induce large pores in the thrombus surface. The high rates of clot mass loss and the obvious changings of fibrin structure make our NUSCA a promising tool for sonothrombolytic therapy 3).