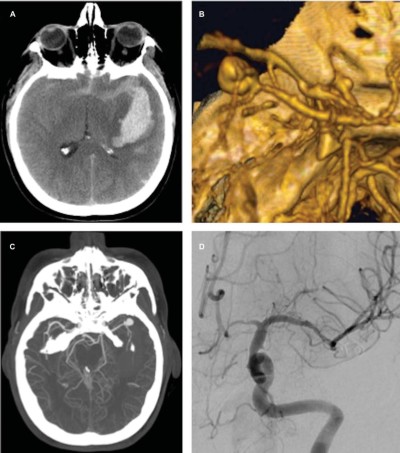
Ruptured middle cerebral artery aneurysm
Microsurgical clipping of ruptured middle cerebral artery aneurysm has several advantages over endovascular treatment, including durability over time. Mooney et al., report detailed outcome data of patients with ruptured MCA aneurysms who underwent microsurgical clipping as part of a prospective, randomized trial. These results should be used for comparison with future endovascular and surgical series to ensure that the best results are being achieved for patients with ruptured MCA aneurysms 1).
Case series
2018
Mooney et al., report a detailed post hoc analysis of ruptured MCA aneurysms treated by microsurgical clipping from the Barrow Ruptured Aneurysm Trial (BRAT).
The cases of patients enrolled in the BRAT who underwent microsurgical clipping for a ruptured middle cerebral artery aneurysm were reviewed. Characteristics of patients and their clinical outcomes and long-term angiographic results were analyzed.
Fifty patients underwent microsurgical clipping of a ruptured MCA aneurysm in the BRAT, including 21 who crossed over from the endovascular treatment arm. Four patients with nonsaccular (e.g., dissecting, fusiform, or blister) aneurysms were excluded, leaving 46 patients for analysis. Most (n = 32; 70%) patients presented with a Hunt and Hess grade II or III subarachnoid hemorrhage, with a high prevalence of intraparenchymal blood (n = 23; 50%), intraventricular blood (n = 21; 46%), or both. At the last follow-up (up to 6 years after treatment), clinical outcomes were good (modified Rankin Scale score 0-2) in 70% (n = 19) of 27 Hunt and Hess grades I-III patients and in 36% (n = 4) of 11 Hunt and Hess grade IV or V patients. There were no instances of rebleeding after the surgical clipping of aneurysms in this series at the time of last clinical follow-up.
Microsurgical clipping of ruptured MCA aneurysms has several advantages over endovascular treatment, including durability over time. The authors report detailed outcome data of patients with ruptured MCA aneurysms who underwent microsurgical clipping as part of a prospective, randomized trial. These results should be used for comparison with future endovascular and surgical series to ensure that the best results are being achieved for patients with ruptured MCA aneurysms 2).
2015
The records of 49 patients with ruptured middle cerebral artery aneurysm with large intracranial hematomas treated with hematoma evacuation and aneurysm clipping between January 2000 and December 2013 were retrospectively reviewed.
Within this cohort, 35 patients (71.4%) were Hunt and Hess grade IV or V on presentation. The mean hematoma volume was 100.4 ± 77.2 mL. Craniectomy was performed in 40 patients (81.6%). Angiographic vasospasm developed in 15 patients (30.6%). The in-hospital mortality rate was 28.6% (14 patients). At a mean of 25.3 ± 34.0 months follow-up, a good outcome (modified Rankin Scale [mRS] score 0-3) was observed in 18 patients (36.7%).
Significant factors associated with poor outcome or death (mRS scores of 4-6) included increasing age (P < .01), increasing Hunt and Hess grade (P = .03), increasing modified Fisher grade (P = .01), presence of intraventricular hemorrhage (P < .01), decreasing percentage of hematoma evacuation (P < .05), need for craniectomy (P <. 01), need for external ventricular drainage (P = .04), and angiographic vasospasm (P = .02) 3).
1987
Four women, aged 39 to 46 years, were urgently admitted to our neurosurgical unit after strokes. On admission, all appeared moribund, presenting with deep coma, pupils bilaterally dilated and fixed, decerebrate posture, and markedly abnormal respiratory patterns. Computed tomography revealed subarachnoid hemorrhage with an associated large intracerebral hematoma and pronounced shift of midline structures in all four cases. Because of the clinical appearance, the patients were given urea and were operated without preceding angiography. The origin of the hemorrhage was identified as a middle cerebral artery (MCA) bifurcation berry aneurysm in one patient and giant MCA aneurysms in the other three. The hematomas were evacuated, and the aneurysms were occluded. All four patients received intravenous nimodipine, none showed any sign of delayed ischemic deterioration, and all regained full consciousness within a few days. One patient died 3 weeks later from a pulmonary embolus. Three patients are presently at home with moderate focal neurological deficits and moderate to marked cognitive impairment. The psychosocial readjustment was very good in a patient with a left giant aneurysm, satisfactory in a patient with a right giant aneurysm, and unsatisfactory in a patient with a right berry aneurysm. The indications, ethical considerations, and technical aspects of operating on seemingly moribund patients who probably harbor a ruptured MCA aneurysm are discussed 4).