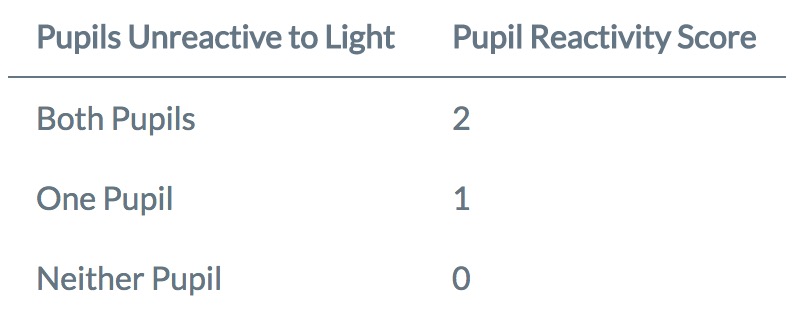
Pupil Reactivity Score
The GCS Pupils Score (GCS-P) was described by Paul Brennan, Gordon Murray and Graham Teasdale in 2018 as a strategy to combine the two key indicators of the severity of traumatic brain injury into a single simple index.
How do I calculate the GCS-P?
The GCS-P is calculated by subtracting the Pupil Reactivity Score (PRS) from the Glasgow Coma Scale (GCS) total score:
GCS-P = GCS - PRS
The Pupil Reactivity Score is calculated as follows.
see more at http://www.glasgowcomascale.org/what-is-gcs-p/
Information about early GCS scores, pupil responses, late outcomes on the Glasgow Outcome Scale, and mortality were obtained at the individual patient level by reviewing data from the CRASH (Corticosteroid Randomisation After Significant Head Injury; n = 9,045) study and the IMPACT (International Mission for Prognosis and Clinical Trials in TBI; n = 6855) database. These data were combined into a pooled data set for the main analysis.
Methods of combining the Glasgow Coma Scale and pupil reaction data varied in complexity from using a simple arithmetic score (GCS score [range 3-15] minus the number of nonreacting pupils [0, 1, or 2]), which Brennan et al., called the GCS Pupils score (GCS-P; range 1-15), to treating each factor as a separate categorical variable. The content of information about patient outcome in each of these models was evaluated using Nagelkerke R2.
Separately, the GCS score and pupil response were each related to outcome. Adding information about the pupil response to the GCS score increased the information yield. The performance of the simple GCS-P was similar to the performance of more complex methods of evaluating traumatic brain damage. The relationship between decreases in the GCS-P and deteriorating outcome was seen across the complete range of possible scores. The additional 2 lowest points offered by the GCS-Pupils scale (GCS-P 1 and 2) extended the information about injury severity from a mortality rate of 51% and an unfavorable outcome rate of 70% at GCS score 3 to a mortality rate of 74% and an unfavorable outcome rate of 90% at GCS-P 1. The paradoxical finding that GCS score 4 was associated with a worse outcome than GCS score 3 was not seen when using the GCS-P.
A simple arithmetic combination of the GCS score and pupillary response, the GCS-P, extends the information provided about patient outcome to an extent comparable to that obtained using more complex methods. The greater range of injury severities that are identified and the smoothness of the stepwise pattern of outcomes across the range of scores may be useful in evaluating individual patients and identifying patient subgroups. The GCS-P may be a useful platform onto which information about other key prognostic features can be added in a simple format likely to be useful in clinical practice 1).