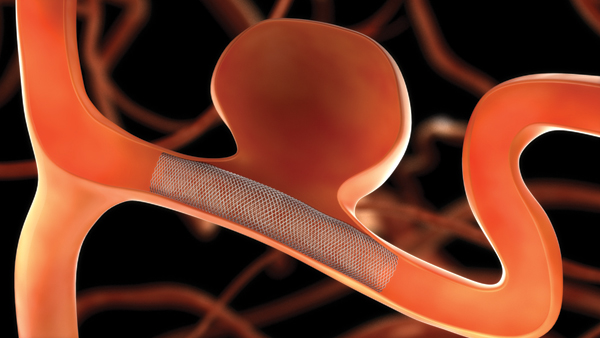
Pipeline
Dispositivo de embolización de Covidien para el aneurisma intracraneal gigante.
Se ha descrito la hemorragia cerebral tardía cuya relación sigue siendo poco clara.
En los análisis histopatológicos de las secciones del cerebro a partir de 3 pacientes en los que se desarrollaron hemorragias intracerebrales ipsilaterales se sugiere una posible asociación con la presencia de émbolos de polivinilpirrolidona 1).
1)
Hu YC, Deshmukh VR, Albuquerque FC, Fiorella D, Nixon RR, Heck DV, Barnwell
SL, McDougall CG. Histopathological assessment of fatal ipsilateral
intraparenchymal hemorrhages after the treatment of supraclinoid aneurysms with
the Pipeline Embolization Device. J Neurosurg. 2013 Dec 10. [Epub ahead of print]
PubMed PMID: 24320006.