Morel-Lavallée lesion
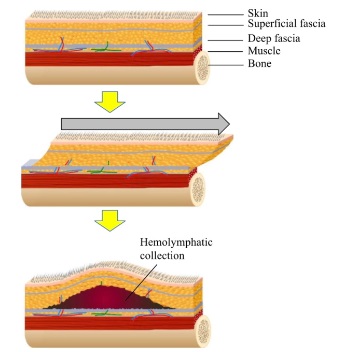
A Morel-Lavallée lesion is a relatively rare condition that occurs when there is a separation or detachment of the skin and subcutaneous tissue from the underlying muscle fascia. This usually happens as a result of a severe blunt trauma or crushing injury, such as in a motor vehicle accident or a fall from a height. The condition is most commonly seen in the hip and thigh area, but can also occur in the lumbar region, as in the case of a lumbar Morel-Lavallée lesion.
The injury can lead to a collection of fluid and blood (hemolymph) within the space created by the separation of tissues. This fluid-filled cavity is known as a Morel-Lavallée lesion. The lesion can be painful and is usually characterized by a soft, fluctuant mass on the skin.
Epidemiology
More frequent in young men, lumbar Morel-Lavallée lesion is underdiagnosed.
Complications
In some cases, the lesion may become infected and can lead to serious complications if left untreated.
Treatment
Treatment for a Morel-Lavallée lesion typically involves drainage of the fluid collection, followed by compression therapy to help the skin and tissue adhere back to the underlying fascia. In severe cases, surgery may be necessary to remove the lesion or to repair any damaged tissues. Early diagnosis and treatment is important to prevent complications and to promote optimal recovery.
Lumbar Morel-Lavallée lesion
More frequent in young men, lumbar Morel-Lavallée lesion is underdiagnosed. Thus, there is no consensus on its treatment. However, conservative management followed by close monitoring is advisable in the acute phase. Other therapy includes surgery with or without the use of sclerosing agents. Early diagnosis prevents infections. Although the diagnosis is clinical, magnetic resonance imaging is the critical paraclinical examination for its assessment. The case is interesting because it occurs in a woman following polytrauma, it is an extremely rare lesion, especially in women 1).
Case reports
A 35-year-old African woman was involved in a motor vehicle accident. Physical examination at the emergency department revealed moderate head trauma, a lumbar inflammatory mass, and a closed leg fracture. She underwent a whole-body computed tomography scan, which revealed a left frontalbrain contusion and a large left paraspinal mass in favor of a lumbar Morel-Lavallée lesion. She benefited from osteosynthesis and conservative management of the cerebral and lumbar lesions. After 4 days, she complained of headaches and vomiting. Magnetic resonance imaging was requested. There was resorption of the cerebral contusion, and the lumbar mass was heterogeneous. She was discharged 10 days later without lower back pain and fully recovered from the headaches. Ultrasound of the lumbar soft tissue performed a month later showed no more collection.
More frequent in young men, lumbar Morel-Lavallée lesion is underdiagnosed. Thus, there is no consensus on its treatment. However, conservative management followed by close monitoring is advisable in the acute phase. Other therapy includes surgery with or without the use of sclerosing agents. Early diagnosis prevents infections. Although the diagnosis is clinical, magnetic resonance imaging is the critical paraclinical examination for its assessment. The case is interesting because it occurs in a woman following polytrauma, it is an extremely rare lesion, especially in women 2).
An isolated Morel-Lavallée lesion of the lumbar spine after delayed presentation. In addition to thorough irrigation, debridement, and pseudo-capsulectomy, surgical management included transcutaneous transmyofascial bolstering with a progressive tension suturing technique to close the cavity over drains in a “quilting” fashion. This was followed by 6 days of incisional wound vacuum treatment and 13 days of drainage through 2 Jackson-Pratt drains. At 6-month follow-up, the patient noted resolution of pain and return to baseline level of functioning. No evidence of recurrence was noted. The Morel-Lavallée lesion of the low back represents a difficult soft tissue injury to treat with substantial risk of complications and recurrence. Diagnosing and treating physicians should be familiar with common injury mechanisms and clinical presentations, as well as a variety of nonoperative and operative treatment options 3)
An uncommon case of a chronic Morel-Lavallée lesion in the sacrococcygeal area, a rarely reported location, with an associated coccygeal fracture and dislocation 4)
Two cases that demonstrate a previously unrecognised association of the MLL with thoracolumbar spine fractures. The lesion is frequently missed, or its significance is overlooked, on initial evaluation. Awareness of this injury should allow tailored strategies to decrease the high risk of wound complications 5).
A 45-year old man with voluminous lumbar MLL initially misdiagnosed 6).