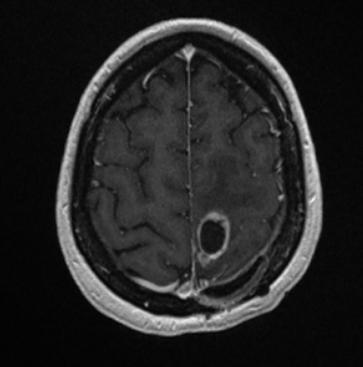
Glioblastoma multiforme in the motor area
J.Sales-Llopis; P.Gonzalez López; I. Verdú Martinez; I. Palomar
Neurosurgery Department, University General Hospital of Alicante, Foundation for the Promotion of Health and Biomedical Research in the Valencian Region (FISABIO), Alicante, Spain
Glioblastoma multiforme is predominantly localized in the cerebral hemisphere, in 24% in and directly around the motor area 1).
Glioblastoma multiforme in the motor area is the surgical challenge because of the need for more radical resection in order to extend the life of the patient, and the risk that radicalism could lead to additional neurological deficit.
Surgery of lesions localized in the motor cortex is a challenging part because of the accompanying risk of de novo occurrence of motor dysfunction.
Intrinsic brain tumors may affect cortical and subcortical structures, with no signs of functional deterioration.
Although the strategy of maximal safe resection is widely accepted, the rates of complete resection of the contrast enhancement tumor (CRET) and the exact causes for motor deficits (mechanical vs vascular) are not always known.
5 aminolevulinic acid combinations
5 aminolevulinic acid and intraoperative magnetic resonance imaging
The combination of 5 aminolevulinic acid (5-ALA) and Intraoperative magnetic resonance imaging, have been proven to increase the rate of CRET, leading resections deeper into the white matter, which in turn endangers neurological function. Balancing the oncological benefit of more extensive resections and the prerequisite of sparing neurological functionality (maximum safe resection) is particularly challenging in patients with glioblastoma close to the corticospinal tract.
5 aminolevulinic acid and intraoperative stimulation mapping
A rather high rate of CRET can be achieved in glioblastomas in motor eloquent areas via a combination of 5 aminolevulinic acid fluorescence guided resection and intraoperative stimulation mapping for distinguishing between presumed and actual motor eloquent tissues. Continuous dynamic mapping was found to be a very ergonomic technique that localizes the motor tissue early and reliably 2).
Preoperative Functional magnetic resonance imaging, neuronavigation for planning the surgical approach and resection margins, intraoperative sonography and 5-ALA guided surgery in combination with the application of intraoperative monitoring (IOM) shows that functional outcome and total to subtotal resection of malignant glioma in the Rolandic region is feasible 3).
5 aminolevulinic acid -intraoperative stimulation mapping in awake patient
Case series
2015
29 patients suffering malignant gliomas in the motor cortex (17) and sensory cortex (12) were analyzed with respect to functional outcome and grade of resections.
Improvement of motor function was seen in 41.5% one week after surgery, 41.5% were stable, only 17% deteriorated. After three months patients had an improvement of motor function in 56%, of Karnofsky Score (KPS) 27% and sensory function was improved in 8%. Deterioration of motor function was seen in 16%, in sensory function 4% and in KPS 28% after three months. 25% showed no residual tumour in early post surgical contrast enhanced MRI. 10% had less than 2% residual tumour and 15% had 2-5% residual tumour.
Preoperative functional neuroimaging, neuronavigation for planning the surgical approach and resection margins, intraoperative sonography and 5-ALA guided surgery in combination with the application of IOM shows that functional outcome and total to subtotal resection of malignant glioma in the Rolandic region is feasible 4).
2012
Bogosavljevic et al. present series of 26 patients with glioblastoma multiforme localized in and around the motor area, who were hospitalized from October 2004 to February 2009. During all operations, they conducted electrostimulation display area of the brain, to the anatomical location of M1 segment of the motor cortex.
Distance of the central sulcus in relation to the coronal suture, measured by magnetic resonance imaging (MRI) was 18.38 mm ± 9.564 mm. The volume of electricity required for a motor response was mean 8.79 ± 1.484 mA, with increasing distance from the coronal suture the amperage required to explicit motor responses decreased. The difference (mm) between the distance from the coronary suture measured using MRI and distances measured electrostimulation smaller and power consumption was less (F = 13.285, p < 0.01).
The method of cortical cerebral cortical stimulation is simple and safe method and a binding protocol to the patient safe operation glioblastoma multiforme localized in the motor area of the brain 5).
Case reports
2013
A 39-year-old man who was operated by a tumor placed into the rolandic area. With the patient anesthetized (propofol+remyfentanil), we performed cortical mapping, neuronavigation and fluorescence-guide resection with 5-aminolevulinic acid. Post-resection neurophysiologic assessment showed a minor and highly localized effect onto the somato-sensory system.
Rolandic area surgery can be safely performed in anesthetized patients when extensive neurophysiological, anatomical and biological assessments are performed 6).