Frontal lobectomy
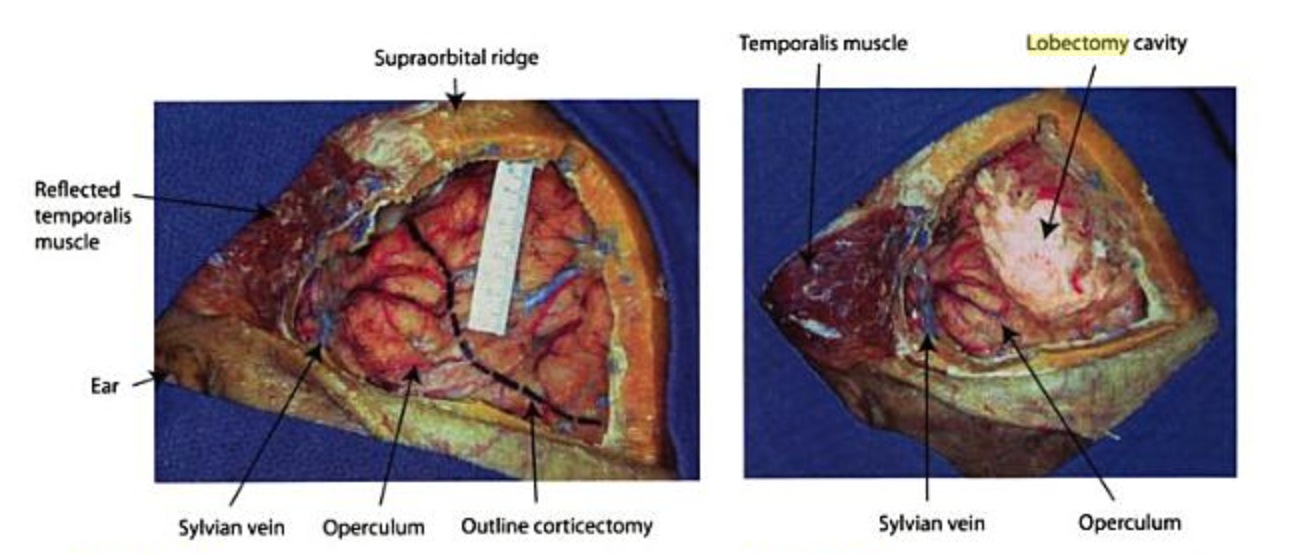 Frontal lobectomy is the removal of a portion of a frontal lobe.
Frontal lobectomy is the removal of a portion of a frontal lobe.
The eloquent boundaries crucial for a safe frontal lobectomy are as follows:
1) the motor cortex
2) the pyramidal tract and premotor cortex in the posterior and posteromedial part of the surgical field
3) the inferior frontooccipital fascicle and the superior longitudinal fasciculus posterolaterally
4) underneath the inferior frontal gyrus, the head of the caudate nucleus, and the tip of the frontal horn of the lateral ventricle in the depth 1).
Indications
Glioma
Reversal of rapid visual loss in a patient with an imaging stable diffuse glioma following frontal lobectomy has been reported 2).
Epilepsy surgery
It is the second most common type of epilepsy surgery, after temporal lobectomy. The success rates for frontal lobectomy are not as good as those for temporal lobectomy: After a frontal lobectomy, 30% to 50% of patients are free of seizures that impair consciousness or cause abnormal movements. 20% to 40% of patients continue to have some complex partial or tonic-clonic seizures but they are reduced by at least 90%. 20% to 30% of patients have no worthwhile improvement. Although the results are not as good as with temporal lobectomy, at least 70% of patients who have had a frontal lobectomy enjoy a great improvement in seizure control. Most patients need to continue taking seizure medicines, but they may need to take less. The frontal lobes are responsible for certain kinds of behavior, and patients who have a frontal lobectomy risk experiencing changes in this behavior. Some problems may have been present before surgery or as a result of seizures in that area. Behaviors that may be affected include: Motivation, attention or concentration Organization and other 'executive functions' Mood, impulse control
Ideal surgical candidates are those in whom there is MRI and electrophysiological evidence of epileptogenicity that is restricted to the frontal lobe, and in whom a complete resection of the epileptogenic zone is possible 3).
Head Injury
Selected severe head injury patients with focal brain lesions and intractable intracranial hypertension or herniation may benefit from brain lobectomies. The survival and functional outcomes after this procedure are acceptable. Blunt trauma, low initial GCS score, and frontal lobectomies are significant risk factors for poor outcomes 4).
Complications
Target detection deficits 5).
