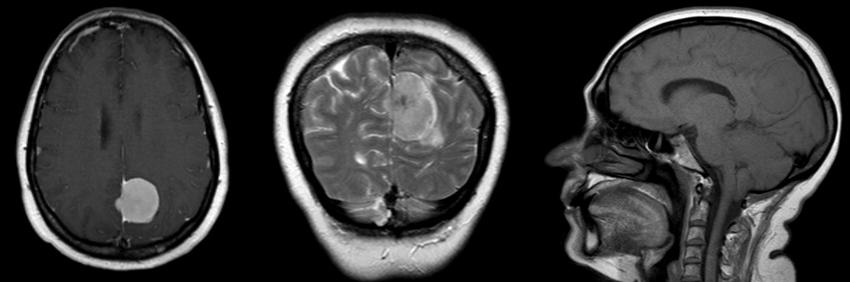
Falcine meningioma of the posterior third
Pablo Gonzalez-Lopez, Paddy Mendez, Patrick Bärtschi, Juan Sales-LLopis, Inmaculada Palomar*
Department of Neurosurgery, General University Hospital Alicante, Spain
*Department of Anesthesiology, General University Hospital Alicante, Spain
Case report
51 year old Woman, who begins with a sudden onset of headache. Conscious, oriented and without neurological deficit
Interhemispheric surgical approach
Meningioma exposure
Falcine meningioma of the posterior third is a type of parasagittal meningioma of the posterior third.
Generally posterior to the sensorimotor strip, may produce focal motor seizures and/or seizures arising from compromise to the visual cortex. If located sufficiently far posteriorly, they may involve the junction of the sagittal sinus with the transverse sinus and adjacent tentorium. In depth those tumors may evolve the incisural notch laterally or posteriorly and attach to the tentorium as a true falcotentorial meningioma, and the removal of these tumors certainly represent a more complex and technical challenge.
For tumors placed posteriorly and in the inferior portion of falx depth, an occipital interhemispheric surgical approach should be tailored to the dural origin and the extent of the tumor as depicted from preoperative MRI. Preservation of the straight sinus and Galenic venous system is always recommended. In those cases, additional resection of the falx and/or incision of the tentorium may be performed with complete resection (Simpson grade 1 and 2) in almost 85% of patients 1).
Case series
4 meningiomas between 1990 and 2010 were analysed retrospectively. Preoperative planning included magnetic resonance imaging (MRI) and magnetic resonance venography (MRV) or angiography.
Visual disturbances and headache were the most commonly referred symptoms
No perioperative deaths or relevant postoperative complications occurred.
Visual function is crucial for clinical outcome. Since an improvement of the deficit might still be possible, every effort should be undertaken to preserve the visual cortex 2).
In 23 patients after operation 20 patients were absolutely able, Rankin score 0, after six months postoperative period (83.3% had excellent results) and no mortality. Resection of sagittal sinus is a factor of a bad outcome, due to cerebral infarction 3).