Kano et al. analyzed 422 consecutive patients (1440 brain metastases) who underwent Gamma Knife radiosurgery (SRS). The median total brain tumor volume was 4.7 cm3 (range 0.3-69.3 cm3), and the median number of metastases was 2 (range 1-32). One hundred thirty-two patients underwent whole brain radiation therapy. Survival times were compared using recursive partitioning analysis (RPA), the Score Index for Radiosurgery (SIR), the Basic Score for Brain Metastases (BSBM), and the Diagnosis Specific Graded Prognostic Assessment (DS-GPA).
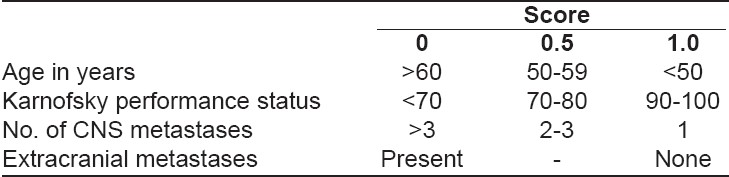
The overall survival times after SRS were compared. With the RPA index, survival times were 2.6 months (Class III, n = 27), 5.5 months (Class II, n = 348), and 13.0 months (Class I, n = 47). With the DS-GPA index, survival times were 2.8 months (Scores 0-1, n = 67), 4.2 months (Scores 1.5-2.0, n = 143), 6.6 months (Scores 2.5-3.0, n = 111), and 9.4 months (Scores 3.5-4.0, n = 101). With the SIR, survival times were 3.2 months (Scores 0-3, n = 56), 5.8 months (Scores 4-7, n = 319), and 12.7 months (Scores 8-10, n = 47). With the BSBM index, survival times were 2.6 months (BSBM0, n = 47), 5.4 months (BSBM1, n = 282), 11.0 months (BSBM2, n = 86), and 8.8 months (BSBM3, n = 7). The DS-GPA index was the most balanced by case numbers in each class and provided the overall best prognostic index for overall survival.
The DS-GPA index proved most balanced and predictive of survival for patients with melanoma who underwent SRS as part of management for brain metastases. Patients whose DS-GPA score was ≥ 2.5 had predictably improved survival times after SRS 1).