Chicago Chiari Outcome Scale
Application of Chicago Chiari Outcome Scale (CCOS) to a larger patient population undergoing a variety of operative Chiari Malformation Type 1 (CM1) treatments should allow for better-informed decisions regarding patient selection and treatment options for CM1 1).
Greenberg et al. searched PubMed, Embase, the Cumulative Index to Nursing and Allied Health Literature, ClinicalTrials.gov , and Cochrane databases to identify publications between January 2003 and August 2013 that met the following criteria: 1) reported clinical outcomes in patients treated for CM-I; 2) were original research articles; 3) included at least 10 patients or, if a comparative study, at least 5 patients per group; and 4) were restricted to patients with CM-I.
Among the 74 papers meeting inclusion criteria, there was wide variation in the outcome methods used. However, all approaches were broadly grouped into 3 categories: 1) “gestalt” impression of overall symptomatic improvement (n=45 papers); 2) postoperative change in specific signs or symptoms (n=20); or 3) results of various standardized assessment scales (n=22). Among standardized scales, 11 general function measures were used, compared with 6 disease-specific tools. Only 3 papers used scales validated in patients with CM-I. To facilitate a uniform comparison of these heterogeneous approaches, the authors appraised articles in multiple domains defined a priori as integral to reporting clinical outcomes in CM-I. Notably, only 7 articles incorporated patient-response instruments when reporting outcome, and only 22 articles explicitly assessed quality of life.
The methods used to evaluate clinical outcomes in CM-I are inconsistent and frequently not comparable, complicating efforts to analyze results across studies. Development, validation, and incorporation of a small number of disease-specific patient-based instruments will improve the quality of research and care of CM-I patients 2).
The development of the Chicago Chiari Outcome Scale and the Chiari Symptom Profile provides CM-I-specific instruments to measure outcomes in adults and children, although validation and refinement may be necessary 3).
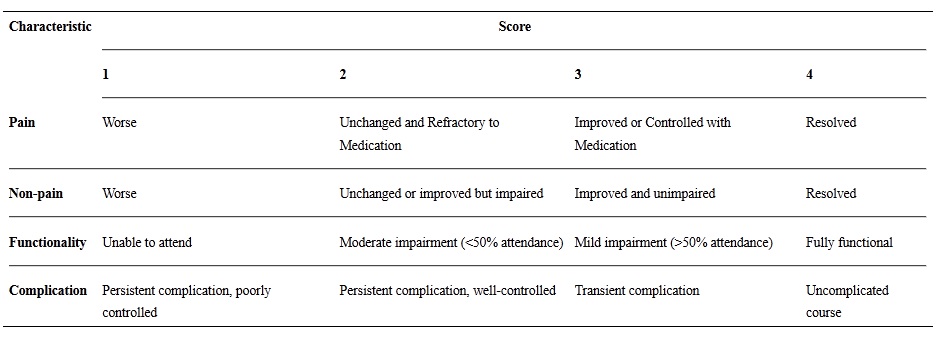
The Chicago Chiari Outcome Scale (CCOS) uses 4 postoperative outcome categories (pain, nonpain symptoms, functionality, and complications) graded 1 to 4 for a total possible score of 16. As a comparison with current Chiari outcome methodology, each patient was also placed into a gestalt outcome group of “improved,” “unchanged,” or “worse” (I/U/W). Patients were stratified by CCOS scores and by I/U/W group.
Stratifying patients by total CCOS scores showed that patients who achieved CCOS scores between 13 and 16 were predominantly in the I/U/W improved group (n = 101, 69%); scores between 9 and 12 were predominantly I/U/W unchanged (n = 39, 27%), and scores between 4 and 8 were I/U/W worse (n = 6, 4%). Symptom subscore results provided insight into the specifics of the overall outcome in addition to the more quantitative nature of the 16-point scale 4)
In a external validation study, the CCOS was effective at identifying patients with improved outcomes and proved more reliable than the authors' gestalt impression of outcome. However, certain component subscores (functionality and nonpain symptoms) were found to be less reliable, and may benefit from further definition in score assignment. In particular, the functionality subscore does not add to the predictive ability of the CCOS, and may be unnecessary. Overall, the authors found the CCOS to be an improvement over the previously used assessment of outcome at their institution 5).
In retrospectively reviewed records of 36 patients treated with PFDD and 29 patients with PFDO between 2003 and 2011. Lee et al. compared baseline demographic, clinical, and radiographic characteristics. The primary clinical outcome was the Chicago Chiari Outcome Scale (CCOS). The primary radiographic outcome was qualitative syrinx improvement or resolution 6).
The strongest physiological parameter predictive of outcome was the preoperative maximal cord displacement in the upper cervical region during the cardiac cycle, which was significantly larger in the favorable-outcome subcohorts for both outcome types (p < 0.05). Several hydrodynamic measures revealed significantly larger preoperative-to-postoperative changes in the favorable-outcome subcohort. Predictor sets for the chief-complaint classification included the cord displacement, percent venous drainage through the jugular veins, and normalized cerebral blood flow with 93.3% accuracy. Maximal cord displacement combined with intracranial volume change predicted outcome based on the modified CCOS classification with similar accuracy. CONCLUSIONS Tested physiological measures were stronger predictors of outcome than the morphological measures in patients with CM-I. Maximal cord displacement and intracranial volume change during the cardiac cycle together with a measure that reflects the cerebral venous drainage pathway emerged as likely predictors of decompression outcome in patients with CM-I 7).