Brainstem Cavernous Malformation Case Series
Four hundred sixty-eight patients (217 female, 46.4%) were included in a study with a median follow-up duration of 79.0 months. A total of 137 prospective hemorrhages occurred in 107 patients (22.9%) during 1854.0 patient years. Multivariate Cox regression analysis found age ≥ 55 years (hazard ratio (HR) 2.166, p = 0.002), Developmental Venous Anomaly (DVA) (HR 1.576, p = 0.026), superficial-seated location (HR 1.530, p = 0.047), and hemorrhage on admission (HR 2.419, p = 0.026) as independent risk factors for hemorrhage. The 5-year cumulative hazard of hemorrhage was 30.8% for the overall cohort, 47.8% for 60 patients with age ≥ 55 years, 43.7% for 146 patients with DVA, and 37.9% for 272 patients with superficial-seated lesions, and 37.2% for 341 patients with hemorrhage on admission. As a stratified analysis, within subcohort of 341 patients with a hemorrhagic presentation, age ≥ 55 years (HR 3.005, p < 0.001), DVA (HR 1.801, p = 0.010), and superficial-seated location (HR 2.276, p = 0.001) remained independently significant. The 5-year cumulative hazard of hemorrhage was 52.0% for 119 patients with both DVA and hemorrhagic presentation. The 5-year cumulative hemorrhagic risk was 30.8% and was higher in subgroups if harboring risk factors that helped to predict potential hemorrhagic candidates and were useful for treatment decision-making.Clinical Trial Registration-URL: http://www.chictr.org.cn Unique identifier: ChiCTR-POC-17011575 1).
2019
DTT findings were evaluated bilaterally for fiber tract displacement or deviation, deformation and interruption in every patient before and after the surgery. Neurological examination was performed at admission, discharge and outpatient follow-up visit. The sensitivity, specificity, positive predictive value and negative predictive values of DTT were calculated both pre- and post-operatively.
There were 25 patients (9 men 16 women) with a mean age of 39.5±13.9 years. The mean size of the CMs was 6909±8374 mm3 (range: 180 mm3-38220 mm3) The mean follow-up time was 42.7±23.2 months (range: 8 to 112 months). Pre-operatively, the sensitivity, specificity, positive and negative predictive values of DTT for corticospinal tracts (CST) and medial lemnisci (ML) were 100%, 60%, 38.4%, 100% and 87.5%, 11.7%, 31.8%, 66.6%, respectively. Post-operatively, the sensitivity, specificity, positive and negative predictive values of DTT for CSTs and ML were 100%, 64.7%, 40%, 100% and 100%, 0%, 33.3%, 66.6%, respectively.
Positive findings on DTT such as fiber tract deviation, deformation, disruption or interruption should be taken cautiously before drawing conclusions of clinically relevant damage of white matter tracts 2).
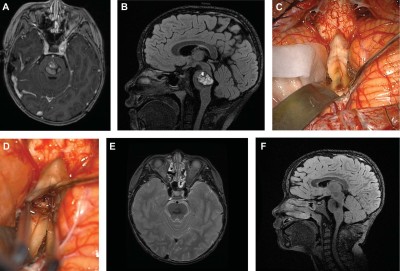
A retrospective review of 46 consecutive cases of BSCMs, with their clinical and radiographic data, was performed. Nine cases were selected to illustrate 7 different operative approaches, and discuss surgical nuances of the less-invasive technique unique to each.
Postoperative morbidity, defined as an increase in modified Rankin Scale, was observed in 5 patients (10.9%). A residual BSCM was present in 2 patients (4.3%); both underwent reoperation to remove the remainder. At follow-up of 31.1 ± 27.8 mo, 3 patients experienced recurrence (6.5%). Overall, 65% of our patients improved, 20% stayed the same, and 11% worsened postsurgery. Two patients died, yielding a mortality of 4.3%.
Using the less-invasive resection technique for piecemeal BSCM removal, in appropriately selected patients, has yielded comparable to improved patient outcomes over existing large series. Lateral, anterolateral, and posterolateral approaches are favorable over direct midline (dorsal or ventral) approaches. A thorough understanding of brainstem safe entry zones, in conjunction with appropriate approach selection, is key to a good outcome in challenging cases 3).
2015
Consecutive patients with brainstem cavernomas who underwent surgical removal from June 2007 to December 2014 were retrospectively analysed. Transcranial motor-evoked potential (MEP) and somatosensory-evoked potential (SSEP) monitorings were performed in all cases. The evoked potential (EP) monitoring data were reviewed and related to new postoperative motor and sensory deficits and postoperative imaging. Clinical outcomes were assessed during follow-up.
Twenty-six consecutive patients with brainstem cavernoma underwent 27 surgical resections within this study. MEP and SSEP monitoring was technically feasible in 26 and 27 cases, respectively. MEP sensitivity and specificity were 33 and 88 %, respectively. MEP positive and negative predictive values were 28 and 78 %, respectively. SSEP sensitivity and specificity were 20 and 81 %, respectively. SSEP positive and negative predictive values were 20 and 81 %, respectively 4)
 A consecutive, single-surgeon series of 104 patients was used to assess preoperative clinical and imaging predictors of microsurgical outcomes. Univariable logistic regression identified predictors and a multivariable logistic regression model tested the association of the combined predictors with final modified Rankin Scale scores. A grading system assigned points for lesion size, location crossing the brainstem's midpoint, presence of developmental venous anomaly, age, and time from last hemorrhage to surgery.
A consecutive, single-surgeon series of 104 patients was used to assess preoperative clinical and imaging predictors of microsurgical outcomes. Univariable logistic regression identified predictors and a multivariable logistic regression model tested the association of the combined predictors with final modified Rankin Scale scores. A grading system assigned points for lesion size, location crossing the brainstem's midpoint, presence of developmental venous anomaly, age, and time from last hemorrhage to surgery.
Average maximal diameter of BSCMs was 19.5 mm; 50% crossed the axial midpoint; 54.8% had developmental venous anomalies; mean age was 42.1 years; and median time from last hemorrhage to surgery was 60 days. One patient died (0.96%), and 15 patients (14.4%) experienced worsened cranial nerve or motor dysfunction, of which 10 increased their modified Rankin Scale scores (9.6%). BSCM grades ranged from 0 to 7 points and predicted outcomes with high accuracy (receiver operating characteristic = 0.86, 95% confidence interval: 0.78-0.94) 5).
Maurer et al. present case series of patients who underwent surgical resection of brainstem cavernous malformations using minimally invasive approaches at our institution from January 2012 to August 2014, all of whom had experienced at least one hemorrhage prior to presentation. Approach choice was determined by location of the cavernous malformation in relation to the brainstem surface. Postoperatively, there were three instances of transient neurologic symptoms, all of which resolved at time of last follow-up. All eight patients experienced neurologic improvement after surgery, with four patients showing no deficits at last follow-up. Approach selection rationale and technical nuances are presented on a case-by-case basis. With carefully planned keyhole approaches to cavernous malformations presenting to the brainstem surface, excellent results may be achieved without the necessity of larger conventional craniotomies. They believe the nuances presented may be of use to others in the surgical treatment of these lesions 6).
2010
36 consecutive patients (12 men, 24 women; mean age, 42 years) who underwent microsurgical resection of brainstem cavernomas between 1996 and 2006. Medical records, surgical records, and neuroimaging examinations were evaluated. All 36 patients presented with > or =1 hemorrhage from the cavernomas and preoperatively displayed some neurological symptoms. Surgical approach was midline suboccipital for 16 pontine and/or medullary cavernomas under the floor of the fourth ventricle, retrosigmoid for 10 lateral mesencephalic, pontine, and/or medullary cavernomas, occipital transtentorial approach for 2 thalamomesencephalic and 3 mesencephalic cavernomas, combined petrosal for 2 pontine cavernomas, and other for 3 cavernomas. Complete resection according to postoperative magnetic resonance imaging was achieved in 33 of 36 patients. No mortality was encountered in this study. New neurological deficit occurred in the early postoperative period for 18 patients, but was transient in 15 of these. Neurological state as of final follow-up was improved in 16 patients (44%), unchanged in 17 (47%), and worsened in 3 (8%) compared with preoperatively. In conclusion, symptomatic brainstem cavernomas should be considered for surgical treatment. Careful selection of the optimal operative approach and a meticulous microsurgical technique are mandatory 7).
1991
Twenty-four patients with long-tract and/or cranial nerve findings from their cavernous malformations of the brain stem were seen for initial evaluation or surgical consultation and thereafter received either surgical or continued conservative treatment. The decision to operate was based on the proximity of the cavernous malformation to the pial surface of the brain stem, the patient's neurological status, and the number of symptomatic episodes. Sixteen patients were treated by definitive surgery directed at excision of their malformation. In four patients, associated venous malformations influenced the surgical approach and their recognition avoided the risk of inappropriate excision of the venous malformation. Although some of the 16 patients had transient, immediate, postoperative worsening of their neurological deficits, the outcome of all except one was the same or improved. Only one patient developed recurrent symptoms: a new deficit 2 1/2 years after surgery required reoperation after regrowth of the cavernous malformation. She has been neurologically stable since the second surgery. One patient died 6 months postoperatively from a shunt infection and sepsis. The eight conservatively treated patients are followed with annual magnetic resonance imaging studies. One has a dramatic associated venous malformation. Seven patients have either minor intermittent or no symptoms, and the eighth died from a hemorrhage 1 year after his initial presentation. Based on these results, surgical extirpation of symptomatic cavernous malformations of the brain stem appears to be the treatment of choice when a patient is symptomatic, the lesion is located superficially, and an operative approach can spare eloquent tissue. When cavernous malformations of the brain stem are completely excised, cure appears permanent 8).