AOSpine thoracolumbar spine injury classification system
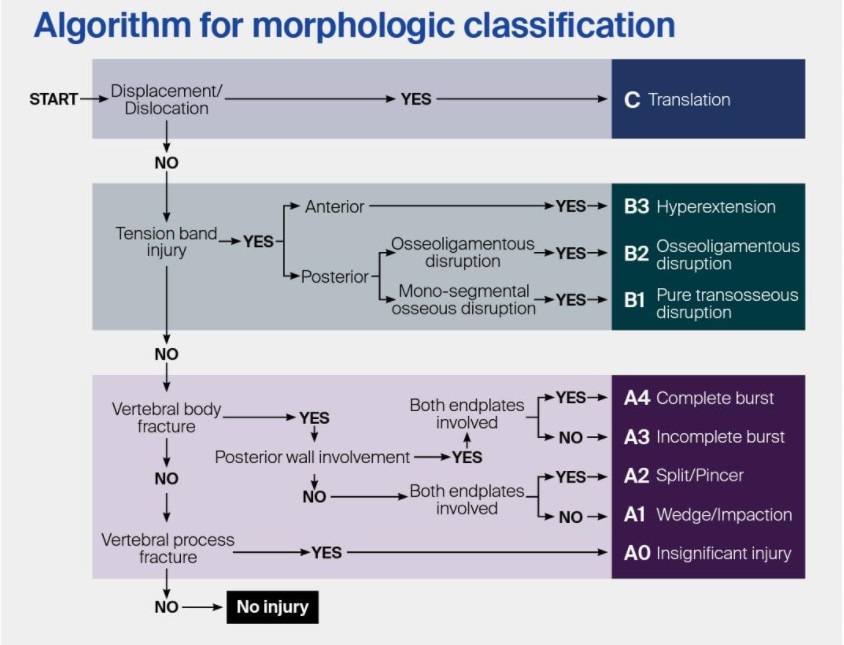
Picture: AOSpine thoracolumbar spine injury classification system
see also Thoracolumbar spine fracture classification.
This classification allows adequate agreement among different observers and by the same observer on separate occasions 1).
The AOSpine thoracolumbar and subaxial cervical spine injury systems show substantial reliability, thus being valuable tools for clinical and research purposes 2).
The reliability of the AOSpine fracture classification is superior to the TLICS and the LSC. Therefore, this classification system could best be applied within clinical practice 3).
Given a lack of a uniform classification in the pediatric population, the AOSpine thoracolumbar spine injury classification system has the potential to be used as the first universal spine fracture classification in children 4).
The inter- and intraobserver reliability for the AOSpine Thoracolumbar Spine Injury Classification System was high amongst pediatric orthopedic surgeons. The AOSpine Thoracolumbar Spine Injury Classification System is a promising option as a uniform fracture classification in children 5)
AOSpine thoracolumbar spine injury classification system Subtype A0
AOSpine thoracolumbar spine injury classification system Subtype A1
AOSpine thoracolumbar spine injury classification system Subtype A2
AOSpine thoracolumbar spine injury classification system Subtype A3
AOSpine thoracolumbar spine injury classification system Subtype A4
AOSpine thoracolumbar spine injury classification system Subtype B
AOSpine thoracolumbar spine injury classification system Subtype C
AOSpine thoracolumbar spine injury classification system Subtype C
Historically, classifications focused only on the osseous injuries; more recent classifications focused on the injury morphology and other critical determinants of treatment, including the posterior ligamentous complex integrity and the patient's neurologic status 6).
Although the Magerl classification of thoracolumbar spinal fractures and thoracolumbar injury classification system (TLICS) are both well-known schemes to describe Thoracolumbar spine fractures, no thoracolumbar injury classification system has achieved universal international adoption. This lack of consensus limits communication between clinicians and researchers complicating the study of these injuries and the development of treatment algorithms 7).
A simple and reproducible classification system of TL injuries was developed using a structured international consensus process. This classification system consists of a morphologic classification of the fracture, a grading system for the neurological status, and description of relevant patient-specific modifiers. Forty cases with a broad range of injuries were classified independently twice by group members 1 month apart and analyzed for classification reliability using the Kappa coefficient (κ).
The morphologic classification is based on 3 main injury patterns: type A (compression), type B (tension band disruption), and AOSpine Thoracolumbar type C fracture (displacement/translation) injuries. Reliability in the identification of a morphologic injury type was substantial (κ= 0.72).
The AOSpine TL injury classification system is clinically relevant according to the consensus agreement of our international team of spine trauma experts. Final evaluation data showed reasonable reliability and accuracy, but further clinical validation of the proposed system requires prospective observational data collection documenting use of the classification system, therapeutic decision making, and clinical follow-up evaluation by a large number of surgeons from different countries 8).
A survey was sent to 100 AOSpine members from all 6 AO regions of the world (North America, South America, Europe, Africa, Asia, and the Middle East). Each respondent was asked to numerically grade the severity of each variable of the AOSpine Thoracolumbar Spine Injury Classification System including the morphology, neurological grade, and patient specific modifiers. A grade of zero was considered to be not severe at all, and a grade of 100 was the most severe injury possible.
Seventy-four AOSpine surgeons from all 6 AO regions of the world numerically graded the severity of each variable of the AOSpine Thoracolumbar Spine Injury Classification System to establish the injury severity score. The reported fracture severity increased significantly (P < 0.0001) as the subtypes of fracture type A and type B increased, and a significant difference (P < 0.0001) in severity was established for burst fractures with involvement of 2 versus 1 endplates. Finally, no regional or experiential difference in severity or classification was identified.
Development of a globally applicable injury severity scoring system for thoracolumbar trauma is possible. This study demonstrates no regional or experiential difference in perceived severity or thoracolumbar spine trauma. The AOSpine Thoracolumbar Spine Injury Classification System provides a logical approach to assessing these injuries and enables rational strategies for treatment 9).
Surgeons' experience did not significantly affect overall fracture classification, evaluating stability and planning the treatment. Surgeons with less experience had a higher percentage of correct classification in A3 and A4 injuries. Despite variations between them in classification, the assessment of overall stability and management decisions were similar between the 2 groups 10).
Case series
2017
The AOSpine thoracolumbar spine injury classification system was applied to 109 patients with acute, traumatic thoracolumbar spinal injuries by two groups of spinal surgeons with different levels of clinical experience. The Kappa coefficient was used to determine interobserver reliability and intraobserver reproducibility. RESULTS: The overall Kappa coefficient for all cases was 0.362, which represents fair reliability. The Kappa statistic was 0.385 for A-type injuries and 0.292 for B-type injuries, which represents fair reliability, and 0.552 for C-type injuries, which represents moderate reliability. The Kappa coefficient for intraobserver reproducibility was 0.442 for A-type injuries, 0.485 for B-type injuries, and 0.412 for C-type injuries. These values represent moderate reproducibility for all injury types. The raters in Group A provided significantly better interobserver reliability than Group B (P < 0.05). There were no between-group differences in intraobserver reproducibility.
This study suggests that the new AO spine injury classification system may be applied in day-to-day clinical practice in China following extensive training of healthcare providers. Further prospective studies in different healthcare providers and clinical settings are essential for validation of this classification system and to assess its utility 11).
Clinical and radiological data of 50 consecutive patients admitted at a single centre with a diagnosis of an acute traumatic thoracolumbar spine injury were distributed to eleven attending spine surgeons from six different institutions in the form of PowerPoint presentation, who classified them according to both classifications. After time span of 6 weeks, cases were randomly rearranged and sent again to same surgeons for re-classification. Interobserver and intraobserver reliability for each component of TLICS and new AOSpine classification were evaluated using Fleiss Kappa coefficient (k value) and Spearman rank order correlation.
Moderate interrater and intrarater reliability was seen for grading fracture type and integrity of posterior ligamentous complex (Fracture type: k = 0.43 ± 0.01 and 0.59 ± 0.16, respectively, PLC: k = 0.47 ± 0.01 and 0.55 ± 0.15, respectively), and fair to moderate reliability (k = 0.29 ± 0.01 interobserver and 0.44+/0.10 intraobserver, respectively) for total score according to TLICS. Moderate interrater (k = 0.59 ± 0.01) and substantial intrarater reliability (k = 0.68 ± 0.13) was seen for grading fracture type regardless of subtype according to AOSpine classification. Near perfect interrater and intrarater agreement was seen concerning neurological status for both the classification systems.
The proposed AOSpine classification has better reliability for identifying fracture morphology than the existing TLICS. Additional studies are clearly necessary concerning the application of these classification systems across multiple physicians at different level of training and trauma centers to evaluate not only their reliability and reproducibility, but also the other attributes, especially the clinical significance of a good classification system 12).
Patients who suffered osteoporotic vertebral fractures (OVFs) between January 2012 and December 2014 underwent consecutive radiological assessments, including measurements of anterior height loss (AHL), posterior height loss (PHL), and the kyphotic angle (KA). The fracture morphology was classified by AOSpine thoracolumbar spine injury classification system. MRI was performed at the initial assessment and the extent of canal encroachment (CE) was calculated in all patients. Follow-up computed tomography (CT) or MRI was performed in patients exhibiting significant height loss in follow-up radiography. The fracture patterns in T1- and T2-weighted MRI were also assessed.
A total of 485 patients visited our institute for treatment of OVFs and 97 were enrolled; 15 were male and 82 were female. The mean age at initial visit was 70.3±14.6years. The initial spinal CE was correlated with the initial PHL and the initial AHL. The follow-up CE was correlated with age, the initial PHL, and the difference between the initial and last PHL (ΔPHL(initial-last)). OVFs with both endplate fractures have a greater tendency of posterior wall collapse than those with single endplate fracture. On initial T1-weighted sagittal MRI, a diffuse low signal change pattern of the fractured vertebra was correlated with PHL. Delayed neurological deficits developed in four patients. These patients underwent surgical intervention.
In patients with simple compression fractures, attention should be paid to the posterior vertebral body and both endplates as well as the T1-weighted MRI findings to allow early detection of spinal canal compromise, which can have devastating consequences 13).