Table of Contents
Cognard classification
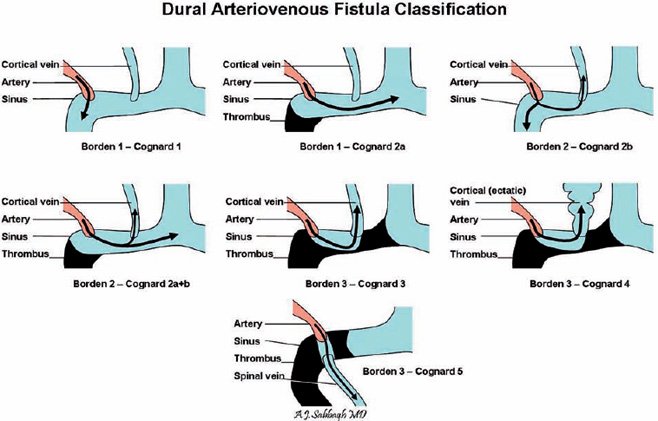
There are numerous Dural arteriovenous fistula classifications. Borden and Cognard are amongst the more widely used.
The Cognard classification of dural arteriovenous fistulas correlates venous drainage patterns with increasingly aggressive neurological clinical course. It was first described in 1995 1).
Probably the most widely used classification system for dural arteriovenous malformations.
Correlates venous drainage patterns with increasingly aggressive neurological clinical course.
Structure
The Cognard classification divides dural arteriovenous fistulas into 5 types according to the following features:
location of fistula
presence of cortical venous drainage
direction of flow
presence of venous ectasia
An alternative classification system is the Borden classification proposed in 1995, which although a little simpler (only 3 grades) does not capture differences which exist in terms of rate of haemorrhage reflected in the Cognard classification. 2) 3)
Type I - confined to venous sinus wall, typically after thrombosis.
Type II
IIa - confined to sinus with reflux (retrograde) into sinus but not cortical veins
Cognard Type IIb dural arteriovenous fistula
Drains into sinus with reflux (retrograde) into cortical veins (10-20% haemorrhage)
Type III - drains direct into cortical veins (not into sinus) drainage (40% haemorrhage)
Type IV - drains direct into cortical veins (not into sinus) drainage with venous ectasia (65% haemorrhage)
Outcome
In terms of prognosis, fistulas can be divided broadly into benign and aggressive lesions as follows:
benign = types I and IIa (lack of cortical venous drainage)
aggressive = everything else
annual risk of non-hemorrhage neurological deficit = 6.9%
annual risk of intracranial hemorrhage = 8.1%
combined annual mortality rate = 10.4% 4).