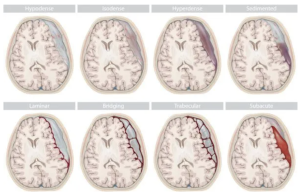
In a review Zhou et al. published in Neurosurgery clinics of North America the most common pulmonary complications following traumatic brain injury (TBI) and spinal cord injury (SCI) — such as neurogenic pulmonary edema, Acute Respiratory Distress Syndrome, Ventilator-Associated Pneumonia, and thromboembolic events — and summarize current understanding of their pathophysiology and treatment, with the goal of guiding early recognition and management to improve outcomes in neurotrauma patients 3)
🧨 Verdict: ❝A clinically themed PowerPoint stretched into ten pages. No risk. No depth. No new thought.❞
⚠️ Fundamental Flaws No Original Contribution → This is not a review — it’s a recitation. The article contributes zero new data, no expert algorithm, and no provocative insight into managing a leading cause of secondary injury in neurotrauma.