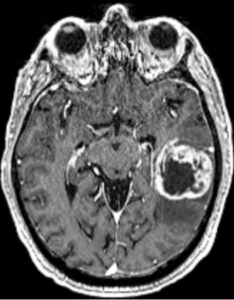
In a retrospective, population-based cohort study with matched controls and longitudinal follow-up, Heinonen et al. from Tampere University Hospital, Helsinki University Hospital, and Harvard Medical School in the Neurosurgery Journal compared 10-year survival rates and causes of death between patients with traumatic head injuries treated at a university hospital and matched population controls. They aimed to identify factors associated with long-term mortality after TBI.
Patients with head injuries exhibited significantly reduced long-term survival compared to matched controls, even after excluding early mortality. However, patient-related characteristics (e.g., comorbidities, lifestyle factors) — more than injury severity itself — appeared to drive this increased mortality risk.
Notably, even patients without documented TBI (likely mild or undiagnosed) showed decreased survival, suggesting an under-recognized long-term impact of head injury across all severity levels 2).
In this population-based cohort study, the authors track 10-year mortality in over 1,900 patients with head injuries versus 9,600 matched controls. Unsurprisingly, trauma patients die more — especially from alcohol, accidents, and “patient characteristics.” The conclusion? It’s not the injury; it’s the person. This study doesn’t just underdeliver — it underthinks.
🧠 1. Conceptual Cowardice: “Patient Characteristics” as a Black Box
The study’s main conclusion — that patient-related factors, not injury severity, explain increased mortality — is not only reductive but evasive. The term “patient characteristics” serves as a statistical landfill for all the unmeasured, uncontrolled, and misunderstood variables: mental health, addiction, social deprivation, neurobehavioral sequelae… all dumped under one lazy label.
Rather than confront the neuropsychiatric aftermath of head trauma, the authors retreat behind correlational shields.
❝They died because of who they were, not what happened to them.❞ — That’s not science. That’s resignation.