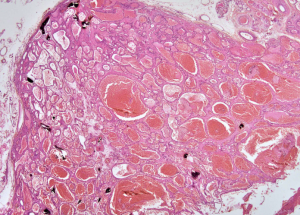
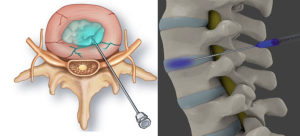
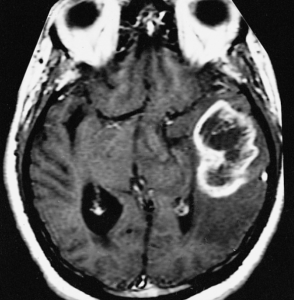
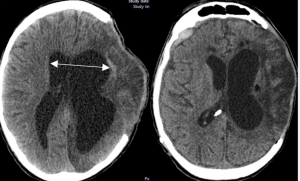
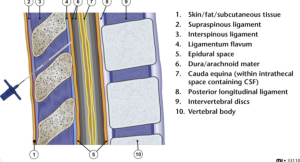
In a case report Hamza Mahdi et al. from the Windsor Regional Hospital, Windsor published in the Journal of medical cases to describe a rare case of intramuscular hemangioma in the lumbar paraspinal region with coexisting L5-S1 disc herniation, and to discuss diagnostic complexities and management strategies. This case underscores the diagnostic challenge of distinguishing benign vascular tumors from other soft tissue lesions in the context of coexisting spinal pathologies. The lesion was misidentified preoperatively despite advanced imaging and biopsy, requiring definitive surgical excision for diagnosis. The authors advocate for the inclusion of vascular tumors in the differential diagnosis of persistent lumbar pain, especially when imaging reveals atypical soft tissue masses 1).
Critical Review
This is the seventh documented adult case of lumbar paraspinal intramuscular hemangioma, lending marginal novelty to the case. The radiologic and histologic evaluation is competently detailed, yet the lack of advanced imaging modalities such as contrast-enhanced MRI or MR angiography limits preoperative characterization. Furthermore, the diagnostic sequence—proceeding to surgery after an inconclusive CT-guided biopsy—reflects a pragmatic yet debatable strategy in light of possible biopsy sampling errors.