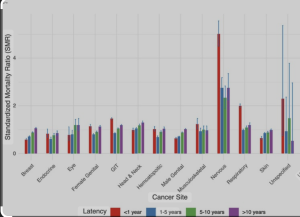
In a retrospective cohort study published in the Journal of Clinical Neuroscience, Ahmed et al. with Cleveland Clinic Cerebrovascular Center, West Virginia University participation 1) analyzed data from over 5.9 million patients diagnosed with a first primary cancer, based on the SEER database (2000–2020). The study aimed to quantify the risk of stroke-related death (SD) in cancer patients and to identify temporal trends and associated clinical and demographic risk factors. Stroke-related mortality (SD) among cancer patients has significantly declined over the past two decades across all cancer types and both sexes. However, older age, non-white race, male sex, and specific cancer types—notably nervous system, respiratory, and head and neck cancers—are associated with a higher risk of stroke death. Conversely, patients receiving chemotherapy or radiotherapy had a lower risk of SD compared to those who received no treatment.
⚠️ Fatal Methodological Flaws
No Clinical Stroke Classification
The authors report on “stroke mortality” without differentiating ischemic vs. hemorrhagic strokes, nor providing stroke etiology or timing relative to cancer diagnosis or cancer treatment—rendering any mechanistic or preventative inference purely speculative.
Reliance on Registry Data Without Validation
The study is built on SEER registry death certificates. These are known to be notoriously unreliable in classifying cause of death in complex patients, particularly in cancer, where the line between terminal illness and stroke is often blurred or misclassified.
Missing Core Clinical Variables
Absolutely no data on cardiovascular comorbidities (e.g., hypertension, atrial fibrillation), medications (e.g., anticoagulants, steroids), or functional status. Without these, attributing causality or understanding modifiable risks is scientifically irresponsible.
“No Treatment” Category is a Black Box
The study repeatedly highlights increased stroke mortality in patients receiving “no treatment”, but never interrogates why. Were they terminal? Frail? Untreated by choice? Refusing care? Without this, comparisons to treated groups are invalid.
Statistical Smoke Without Clinical Fire
The use of large numbers and Annual Percentage Change/SMR modeling creates an illusion of depth. But in the absence of clinical granularity, the findings are epidemiologically flashy and clinically empty.
Cancer Type Associations Are Tautological
Finding increased SD risk in patients with nervous system tumors is hardly surprising, given the direct anatomical involvement. Presenting this as a novel association lacks critical insight and borders on disingenuous.
Temporal Trends Mask Structural Changes
Declines in stroke mortality are presented as a success story—but the study fails to account for changes in diagnostic criteria, coding practices, cancer treatments, and palliative care protocols over 20 years. These are not stable baselines.
🧊 Conclusion: Big Data, Small Insight
This paper is a perfect example of data-driven illusion: a study that rides the wave of big epidemiological numbers without offering a single actionable or mechanistically sound conclusion. It identifies “associations” that are either already known, clinically irrelevant, or artefacts of poor data. The supposed protective effect of chemotherapy/radiotherapy is unadjusted for prognosis, functional status, or therapeutic intent—rendering the headline finding misleading at best.
⚠️ If the purpose of research is to inform practice, this study falls spectacularly short. It tells us what we already suspect, adds confusion where clarity is needed, and fails to bridge data with clinical reality.