In a retrospective secondary analysis based entirely on data from the Global Burden of Disease Study (GBD) 2021 — with no original dataset, no prospective design, and no hypothesis testing — Liu et al., from the Department of Neurosurgery, Heping Hospital Affiliated to Changzhi Medical College, Changzhi, China, published in Frontiers in Cardiovascular Medicine an assessment of the global burden and long-term trends of stroke among young adults (ages 20–39) attributable to metabolic risk factors. The authors identify regional disparities and support the call for targeted prevention strategies.
The study concludes that the global burden of stroke attributable to metabolic risk factors among young adults (20–39 years old) has significantly increased from 1990 to 2021, both in terms of absolute numbers and age-standardized rates. The major contributors to this burden are high body mass index (BMI), high fasting plasma glucose, and high systolic blood pressure. The authors emphasize the need for targeted, age-specific public health interventions to reduce these modifiable risks and prevent early-onset stroke.
Main Limitation
The study merely visualizes model-generated data without offering critical interpretation, clinical insight, or actionable public health strategies.
📉 Main Criticisms
🧮 1. Methodological Cosmeticism
The authors rely exclusively on the GBD model — a black-box statistical engine — without performing sensitivity analyses, falsification tests, or uncertainty quantification beyond what GBD already provides. There is no critical engagement with the source data, regional inconsistencies, or missing datapoints. The paper is a data regurgitation exercise, not a scientific investigation.
📊 2. Descriptive Overload, Analytical Emptiness
The article bombards the reader with numbers (DALYs, ASDR, EAPC, etc.) but offers no mechanistic insight, no new understanding of stroke etiology in young adults, and no translational relevance. It is a prime example of quantitative noise without qualitative understanding.
❌ 3. Misleading Attribution
The term “attributable” is used recklessly to suggest causal relationships between metabolic factors and stroke, despite the fact that GBD data are correlational and model-derived. The authors never address residual confounding, data sparsity, or reverse causation. This amounts to epidemiological overreach.
🧠 4. Neurological Oversimplification
Lumping ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage under one umbrella of “metabolic risk” betrays a lack of pathophysiological literacy. Each stroke subtype has different mechanisms, and the article treats them as interchangeable output rows in a spreadsheet.
🌍 5. Global Epidemiology, Local Irrelevance
Despite invoking 204 countries, the paper ignores healthcare systems, access to care, and sociopolitical determinants. There is no discussion of why Eastern Europe worsens or Sub-Saharan Africa diverges. The result is a shallow cartographic summary with no contextual insight.
🧾 6. Policy Hand-Waving
The conclusions offer generic phrases like “targeted prevention is needed” without any concrete policy proposal, cost-effectiveness model, or health system strategy. This is editorial filler, not policy analysis.
📚 Bottom Line
This paper is a padded PDF version of the GBD stroke dashboard, offering no originality, no clinical guidance, no mechanistic insight, and no policy clarity. It epitomizes the trend of data-driven academic dilution: high-volume output with low-impact substance.
A publication that looks like science, feels like science, but functions like a data echo chamber.
Front Cardiovasc Med. 2025 Jun 2;12:1561052. doi: 10.3389/fcvm.2025.1561052. PMID: 40529554; PMCID: PMC12171433.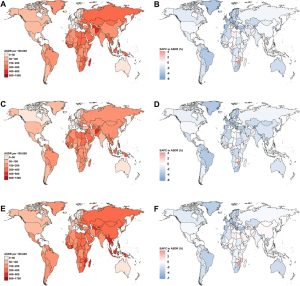
Liu et al. offer a valuable overview of the growing impact of metabolic risk factors on stroke in young adults, using comprehensive GBD 2021 data. The study highlights worrying trends—particularly the rise in stroke-related DALYs driven by high BMI, hypertension, and glucose levels—and emphasizes the need for early prevention.
While the study is descriptive and lacks original data or mechanistic depth, its strength lies in drawing global attention to an under-recognized population: young adults facing preventable vascular risk. The call for targeted interventions is timely, though future work should aim to translate these patterns into actionable, region-specific strategies.
A useful contribution to public health awareness and epidemiological surveillance.