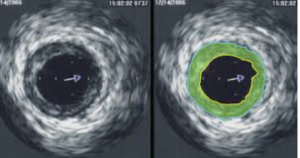
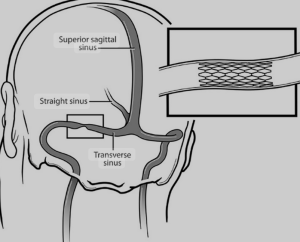
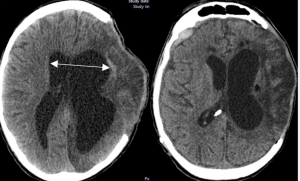
In a retrospective observational pilot study Turpin et al. from the Zucker School of Medicine, Northwell Health, Great Neck, NY published in the Interventional Neuroradiology Journal to assess the utility of intravascular ultrasound (IVUS) versus conventional angiography in quantifying venous sinus stenosis and predicting physiologically significant pressure gradients in patients considered for venous sinus stenting (VSS). IVUS provided higher sensitivity and stronger correlation with manometry-derived pressure gradients than angiography. The authors propose IVUS as a superior, objective adjunct for evaluating VSS candidacy 1).
Critical Appraisal
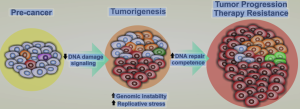
This single-center retrospective analysis of 31 patients compares IVUS to traditional angiography in measuring venous sinus stenosis severity and correlating these with pressure gradients in idiopathic intracranial hypertension (IIH) and pulsatile tinnitus (PT). While the rationale is compelling—addressing known variability in angiographic assessment—the study’s design is inherently limited.