Temporal muscle
The temporal muscle, also known as the temporalis muscle, is a key muscle involved in chewing (mastication). It is located on the side of the skull and is responsible for closing the jaw.
The temporal muscle, also known as the temporalis, is one of the muscles of mastication. It is a broad, fan-shaped muscle on each side of the head that fills the temporal fossa, superior to the zygomatic arch so it covers much of the temporal bone.
Crossing the middle of the parietal bone in an arched direction are two curved lines, the superior temporal line and inferior temporal lines; the former gives attachment to the temporal fascia, and the latter indicates the upper limit of the muscular origin of the temporal muscle.
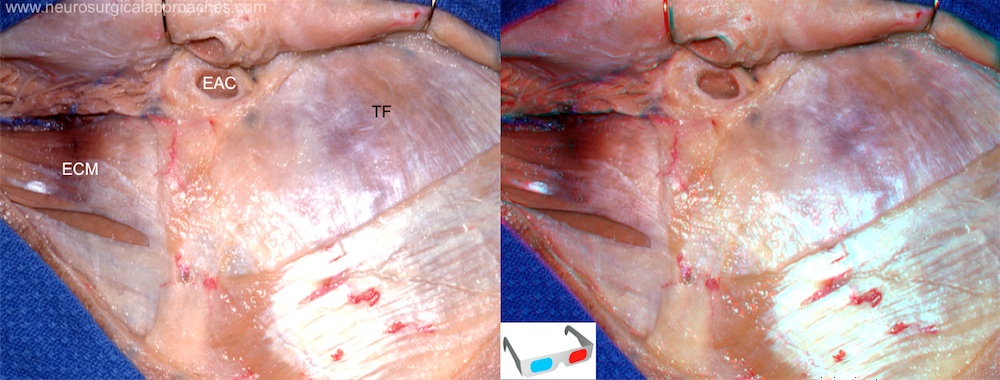
The skin flap is reflected forward to the level of the external auditory canal. The temporal muscle and the sternocleidomastoid muscles are exposed.
EAC: External auditory canal; ECM: Sternocleidomastoid muscle;TF: Temporal fascia.
When Gazi Yasargil first described standard techniques and procedures for pterional craniotomy (PC) in his publication in 1984, subgaleal dissection was used for separation and mobilization of the temporalis muscle. Because subgaleal dissection of the temporalis muscle bears a significant risk of injury to the frontal branches of the facial nerve, various surgical techniques have been adopted such as interfascial dissection and subfascial dissection. However, interfascial dissection is somewhat complex and time-consuming, and, because the facial nerve sometimes courses into the interfascial space, it still cannot eliminate the risk of facial nerve injury. Subfascial dissection is also time-consuming and may result in injury to muscle fibers and intramuscular bleeding. These two techniques require transection of the temporalis muscle to leave a cuff for closure, which causes functional and cosmetic problems by muscle fibrosis and atrophy.
In neurosurgical procedures, avoiding damage of surrounding tissues such as muscle and periosteum during a craniotomy is important for esthetic and other reasons.
Matano et al. devised a protection tool using an amputated syringe barrel to cover the perforating drill and protect temporal muscle damage. This device made it possible to prevent damage to surrounding tissues, such as the muscle and periosteum, during cranial perforation. This method could be useful as it is cost-effective, simple, and versatile 1).
Effect of reflection of temporalis muscle has not been systematically researched. Thirty-nine patients were enrolled to assess the effect of reflection of temporalis muscle during cranioplasty CP after STC. Cranial index of symmetry was adopted to evaluate the aesthetic results, transcranial Doppler was used to assess change of cerebral blood flow (CBF), functional independence measurements were performed to monitor the improvement of neuronal function, and complications associated with CP were also recorded. The results displayed that reflection of temporalis muscle or not had no effect on the anesthetic results. Both operation ways could improve CBF and neuronal function. Cranioplasty with reflection of temporalis muscle could improve CBF and neuronal function more significantly. Furthermore, reflection of temporalis muscle would not increase complications associated with CP. Reflection of temporalis muscle during CP with titanium mesh after STC proves to be an effective and safe operation way 2).
Pterional craniotomy (PC) using myocutaneous (MC) flap is a simple and efficient technique; however, due to subsequent inferior displacement (ID) of the temporalis muscle, it can cause postoperative deformities of the muscle such as depression along the inferior margin of the temporal line of the frontal bone (DTL) and muscular protrusion at the inferior portion of the temporal fossa (PITF). Herein, we introduce a simple method for reconstruction of the temporalis muscle using a contourable strut plate (CSP) and evaluate its efficacy. MATERIALS AND METHODS: Patients at follow-ups between January 2014 and October 2014 after PCs were enrolled in this study. Their postoperative deformities of the temporalis muscle including ID, DTL, and PITF were evaluated. These PC cases using MC flap were classified according to two groups; one with conventional technique without CSP (MC Only) and another with reconstruction of the temporalis muscle using CSP (MC + CSP). Statistical analyses were performed for comparison between the two groups. RESULTS: Lower incidences of ID of the muscle (p < 0.001), DTL (p < 0.001), and PITF (p = 0.001) were observed in the MC + CSP than in the MC Only group. The incidence of acceptable outcome was markedly higher in the MC + CSP group (p < 0.001). ID was regarded as a causative factor for DTL and PITF (p < 0.001 in both). CONCLUSION: Reconstruction of the temporalis muscle using CSP after MC flap is a simple and efficient technique, which provides an outstanding outcome in terms of anatomical restoration of the temporalis muscle 3).
The mini-pterional craniotomy (MPT) provides a reliable and less invasive alternative to the standard pterional craniotomy. Furthermore, ruptured and unruptured anterior circulation aneurysms can safely and effectively be treated with limited bone removal which provides better cosmetic outcomes and excellent postoperative temporalis muscle function 4).
Temporalis muscle volume
Temporal muscle thickness
Chronic craniomandibular pain after craniotomy
Chronic craniomandibular/cervical pain and temporomandibular disorders have not been studied in patients who had a craniotomy several years previously. The aim of the current clinical work was to address these issues.
Methods: A total group of 150 ambulant patients who had a previous craniotomy was subclassified according to whether or not the temporalis muscle was manipulated.
Results: The average incidence of multiple subsite regional head and neck pain was 69.3% a number of years after a craniotomy. Evidence of internal derangement of the temporomandibular joint was significantly higher in the group that required manipulation of the temporalis muscle during the procedure.
Conclusion: The pattern of chronic craniomandibular/cervical pain experienced years after a craniotomy supports the brain neuromatrix theory of pain 5)