Sling retraction technique
A study of Yang et al., from the Department of Neurosurgery, the third hospital affiliated to Soochow, Suzhou Kowloon Hospital Affiliated to Shanghai Jiaotong University School of Medicine, Suzhou. and the Wujin Hospital of Traditional Chinese Medicine, Changzhou, China explored the technical characteristics and effectiveness of sling retraction technique in microvascular decompression for hemifacial spasm.
Between January 2008 and May 2016, 158 patients affected by hemifacial spasm underwent microvascular decompression. Among them, the traditional technique was performed in 86 patients (A Group) and the sling retraction technique was used in 72 patients (B Group). The authors conducted a retrospective study and compared the surgical outcome of the 2 groups. The authors measured cure rate at 3 months and 5 years after microvascular decompression.
In the traditional technique group, the cure rate of microvascular decompression was 94.2% and 83.3%. While in the sling retraction technique group, the cure rate of microvascular decompression was 95.8% and 94.4%. Facial nerve palsy, hearing loss, meningitis, and ataxia were frequent complications in both 2 groups.
The sling technique using biomedical glue is an effective and safe option for patients of hemifacial spasm. During the long-term follow-up, the sling retraction technique of microvascular decompression was more effective than the traditional technique, while there were no significant differences in the incidences of complications 1).
The objectives of a work of Yang et al., of the Department of Neurosurgery, Suzhou Kowloon Hospital, Shanghai Jiaotong University School of Medicine, Suzhou, China are to report the outcomes of the finding during microvascular decompression (MVD) for patients with recurrent trigeminal neuralgia (TN) and to introduce the sling retraction technique.
They performed a retrospective review of redo MVD for consecutive cases with recurrent TN after previous operation. Sling retraction techniques were used during the reoperation.
Fifteen patients underwent redo MVD. During the second operation, arachnoid adhesion of the Teflon felt was confirmed at the trigeminal nerve in 10 cases, and neurovascular conflict was found in 4 cases. Symptoms were completely relieved in 14 patients (93.3%) and partially relieved in 1 patient (6.7%). The mean follow-up period was 38 months (range, 21-60 months), and no patient experienced recurrence.
Arachnoid adhesion of the Teflon felt and vascular compression to the nerve were main causes of recurrence. The sling retraction technique is still an effective and useful treatment for recurrent TN after MVD 2).
Between January 2007 and December 2012, 50 patients with idiopathic TN underwent MVD using the stitched sling retraction technique at the Department of Neurosurgery, Saga, Japan. The median follow-up period was 5.2 years (range, 1.8-6.8 years). Using Kaplan-Meier analysis, the rates of complete pain relief without medications were 88% at 1 year and 83% at 5 years. Recurrence was noted in two patients, and one patient was re-treated using a complementary procedure for pain relief. Although transient complications were observed in seven patients, no permanent neurological deficit was observed. We conclude that the stitched sling retraction technique is a safe and effective treatment for TN and maintains substantial pain relief and low recurrence rates over a long period of time 3).
Swiątnicki et al., from the Department of Neurosurgery, Medical Regional Center, Zgierz, Poland. describe one of the aforementioned modifications that provides a complete and permanent vascular transposition together with its advantages and limitations in the treatment of the hemifacial spasm. Moreover, many aspects of different technical approaches are widely discussed and a case-centered stitched sling retraction technique is presented 4).
3 patients with vertebral artery compression of MO who presented with respiratory failure and/or dysphagia. MVD surgery using the transcondylar fossa approach was effective in relieving patient symptoms.
Although the pathogenic mechanisms of symptomatic vertebral artery compression of MO remain unclear, we should recognize that MVD surgery is effective for selected patients with brainstem dysfunction. The transcondylar fossa approach and the stitched sling retraction technique are appropriate in MVD surgery to relieve vertebral artery compression of MO 5).
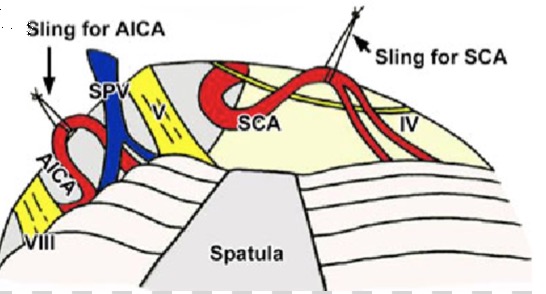
Twelve consecutive patients with recurrent trigeminal neuralgia after previous microvascular decompression(s) were admitted to the Department of Neurosurgery, Imam Khomeini Hospital, Tehran University of Medical Sciences, in Iran form February 2009 to February 2011 and underwent microvascular decompression of the trigeminal nerve using the 'stitched sling retraction' technique. In this technique, the offending loop of the superior cerebellar artery is retracted from the nerve and, using a silk thread loop around it, is suspended to the adjacent tentorium.
All patients experienced pain resolution during the immediate post-operative period or within the first 6 months after surgery. They were followed for 24 to 38 months. No recurrence occurred.
The 'stitched sling retraction' technique shows promising preliminary results in recurrent cases of trigeminal neuralgia after previous microvascular decompression(s). Since it is a 'transposing' technique, it might be associated with less recurrence rates (due to resuming of the neurovascular conflict) than the classic interposing technique, which uses a prosthesis between the offending vessel and the trigeminal nerve 6).
Masuoka et al., reported the stitched sling retraction techniques for treating trigeminal neuralgia (TN), hemifacial spasm (HFS), and glossopharyngeal neuralgia (GPN), focusing on the stitching point for slinging the offending artery in the appropriate direction. Between January 2007 and March 2009, 28 patients with TN, 5 patients with HFS, and 3 patients with GPN underwent MVD with a sling retraction technique. In cases of TN, MVD was performed using the infratentorial lateral supracerebellar approach, and the offending superior cerebellar artery was superomedially transposed with a sling stitched to the tentorium cerebelli. In cases of HFS, MVD was performed using the lateral suboccipital infrafloccular approach, and the offending vertebral artery was superolaterally transposed with a sling stitched to the petrous dura. In cases of GPN, MVD was performed using the transcondylar fossa approach, in which the posterior inferior cerebellar artery was inferolaterally mobilized with a sling secured to the jugular tubercle. No patient suffered recurrence in the follow-up period. For the sling retraction technique to be performed successfully, it is important for a stitch to be placed at a suitable site to sling the offending vessel in the intended direction. An appropriate surgical approach must be used to obtain a sufficient operative field for performing the stitching procedures safely 7).
Fourteen cases of idiopathic GPN were operated on through the transcondylar fossa (supracondylar transjugular tubercle) approach. Their clinical data and operative records were retrospectively reviewed.
In every case, vascular compression on the glossopharyngeal nerve was found and MVD was performed without any major complications. In 13 of the 14 cases the neuralgia completely disappeared postoperatively. Recurrence of pain was found in 1 case. Offending vessels were the posterior inferior cerebellar artery (PICA) in 10 cases, the anterior inferior cerebellar artery (AICA) in 2 cases, and both arteries in 2 cases. In 10 of the 14 cases, the high-origin PICA formed an upward loop between the glossopharyngeal and vagus nerves, compressing the glossopharyngeal nerve upward. In those cases, the PICA was transposed and fixed to the dura mater by the stitched sling retraction technique, and MVD was very effective.
The offending artery was the PICA in most cases. MVD is expected to be very effective, especially when the radiological images show the following 3 findings: 1) high-origin PICA, 2) the PICA making an upward loop, and 3) the PICA coursing the supraolivary fossette. The transcondylar fossa approach is suitable for transposing the PICA by the stitched sling retraction technique, and provides sufficient surgical results 8).
Matsushima et al., reported on Eighty-two patients with trigeminal neuralgia were operated on through microvascular decompression using the technique of interposing Teflon felt between the offending artery and the pons and/or nerve. Recurrence occurred in 14 cases (17.1%) and re-operations were carried out in 6 severe cases at which time the sling retraction technique was used. At the second operation, the adhesion of the interposed Teflon felt was found at the trigeminal nerve in all cases and the adhesions were the main cause of recurrence. The Teflon felt was dissected from the nerve, and the sling of the Teflon felt adhering to the offending arteries was fixed to the tentorium in order to transpose the arteries and avoid re-adhesion. All cases resulted in an excellent relief from pain and experienced no pain for at least 2 years. The intra-operative findings of our cases indicated that the microvascular decompression using the interposing technique may result in adhesion of the prosthesis to the nerve and thus eventually lead to recurrence. Our surgical experience also suggests that such recurrent cases should be re-operated on using the sling retraction technique instead of the interposing technique, even for the first microvascular decompression procedure 9).
He also published the first reported cases in whom the transcondylar fossa approach was applied for the treatment of glossopharyngeal neuralgia (GPN) as a vascular compression syndrome.
All three cases presented with severe paroxysmal pharyngeal pain which could not be controlled by medical treatment. The patients all underwent microvascular decompression surgery (MVD) via transcondylar fossa approach. The posterior inferior cerebellar artery or the anterior inferior cerebellar artery was clearly verified to be compressing the glossopharyngeal nerve and then was safely and completely moved and fixed to the dura mater by the sling retraction technique to effect decompression. No patient has since experienced any further pain or permanent neurological deficit after surgery. TECHNICAL ADVANTAGE: The transcondylar fossa approach is one of the lateral approaches which is different from the transcondylar approach. In this approach, the posterior part of the jugular tubercle is extradurally removed without injuring the atlanto-occipital joint. The entire course of the cisternal portion of the glossopharyngeal nerve can be sufficiently seen with gentle retraction of the cerebellar hemisphere, when using this approach.
This approach makes the MVD for GPN both effective and safe 10).
Melvill and Baxter, from the Mediclinic Constantiaberg, Cape Town, South Africa described a technique whereby a dural sling is fashioned from the tentorium cerebelli , which is used to suspend the vessel away from the nerve and is secured by a single hemoclip 11).