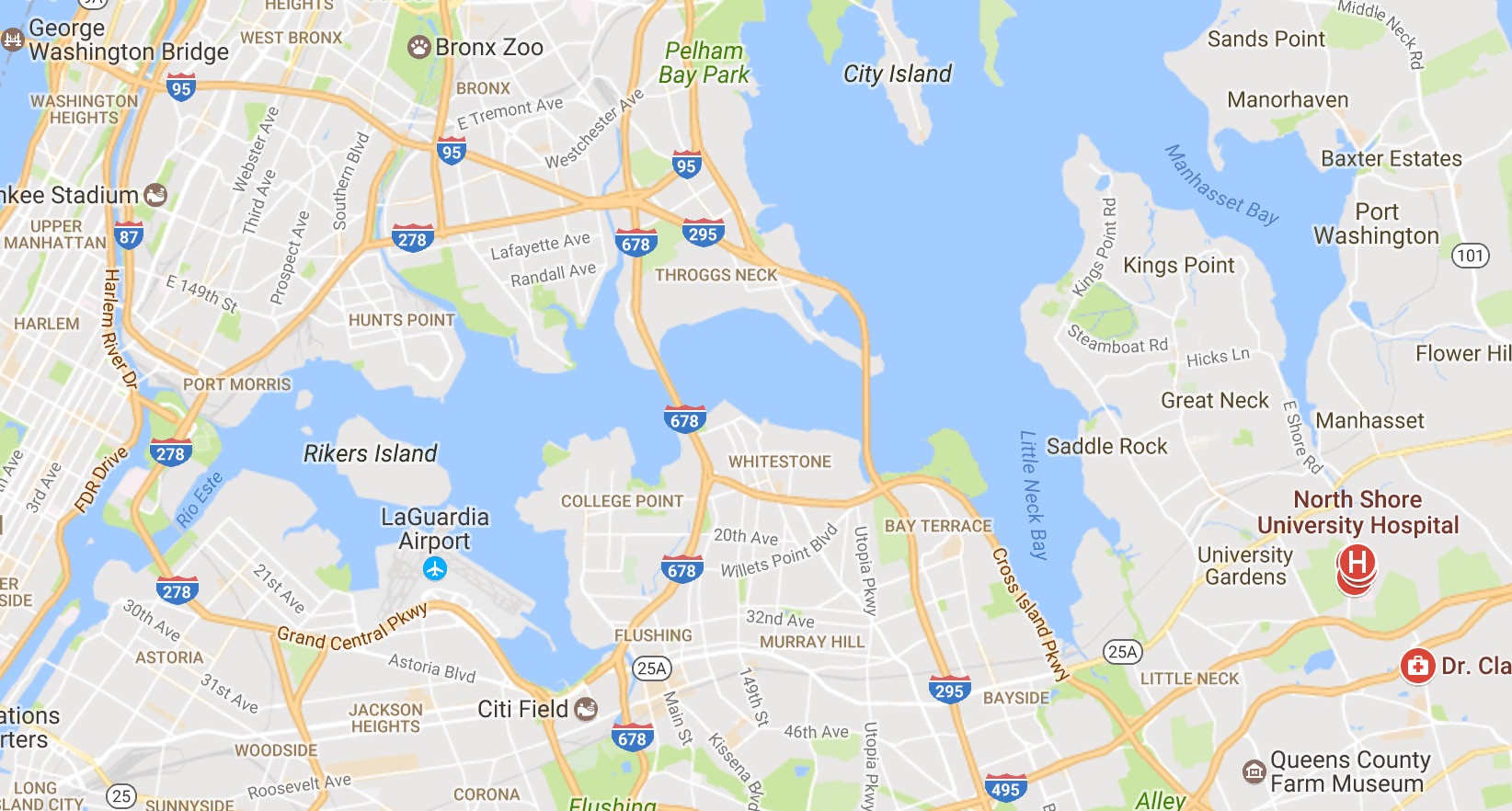
New York City
The Statewide Planning and Research Cooperative System (SPARCS) database was queried to investigate 30-day readmissions and pLOS for transsphenoidal pituitary surgery in New York from 1995 to 2015. Multivariate logistic regression, adjusting for patient and hospital characteristics, was performed to assess the effect of these variables on the outcomes of interest.
A total of 9950 patients underwent transsphenoidal pituitary surgery; 7122 (72%), 2394 (24%), and 434 (4%) patients were treated at high-volume, medium-volume, and low-volume centers, respectively. Patient factors associated with treatment at high-volume centers (HVCs) included: top income quartile, private insurance, urban residence, and white or Asian race (p < 0.05). Patient variables associated with treatment at low-volume centers (LVCs) included: age >65 years, elevated Charlson comorbidity index (CCI) scores, bottom income quartile, Medicaid and Medicare insurance, rural residence, black race, and Hispanic ethnicity (p < 0.05). Variables predictive of prolonged hospitalizations in our multivariable model included black race, Hispanic ethnicity, Medicaid insurance, low income, female gender, LVC, and comorbidities (panhypopituitarism, hypothyroidism, diabetes insipidus [DI], visual disturbances, CCI) while predictors of readmissions included Asian race, female gender, and comorbidities (Cushing syndrome, DI, CCI).
Patients undergoing transsphenoidal pituitary surgery at HVCs have shorter hospitalizations, fewer postoperative electrolyte abnormalities, and lower charges; however, socioeconomic factors may influence access to quality care 1).
Hospitals
Cohen Children's Medical Center
Montefiore Medical Center, Bronx.
Mount Sinai Hospital West.
Department of Neurosurgery, Stony Brook University, Stony Brook, New York, USA
Weill Cornell Medical College.
Department of Neurosurgery, The Center for Stem Cell Biology, Memorial Sloan-Kettering Cancer Center, New York, NY, USA
North Shore University Hospital
Department of Neurosurgery, Hofstra Northwell School of Medicine, and Northwell Health, 300 Community Drive, 9 Tower, Manhasset, NY, USA.
Using a comprehensive all-payer cohort of patients with brain tumors in New York State, Missios and Bekelis identified wide disparities at the hospital and the county level despite comprehensive risk-adjustment. Increased charges were not associated with shorter length of stay (LOS), or lower rates of death and unfavorable discharge 2).