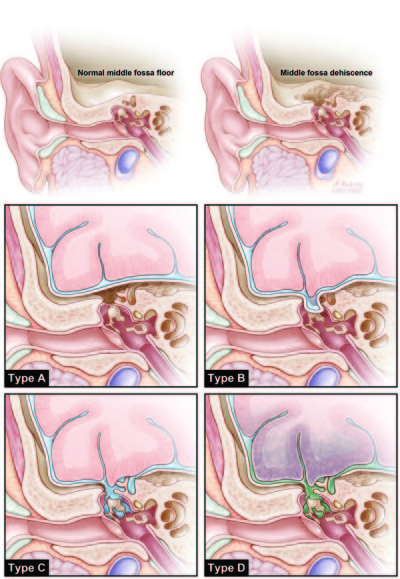
Middle fossa floor dehiscence
Middle fossa floor dehiscence (MFFD) can present as multiple syndromes depending on dehiscence location, tissue herniation, and dural opening.
Classification
Gupta ey al. proposed a classification system for MFFD with the potential to guide clinical decision making.
A retrospective analysis of the electronic medical records (years 1995-2012) of patients who had undergone temporal craniotomy for the surgical repair of an MFFD syndrome at a single institution was undertaken. Reviewed data included demographic, operative, presentation, and outcome details.
Middle fossa floor dehiscence was classified as follows:
Class A, bony dehiscence without herniation of the brain and/or meninges
Class B, herniation of the brain and/or meninges through the middle fossa floor without CSF leakage
Class C, dehiscence with CSF leakage without meningitis
Class D, dehiscence with meningitis.
Case series
2018
A total of 34 patients underwent a total of 37 surgeries. Obesity was prevalent; 21 patients (61.8%) were obese (BMI [body mass index] > 30 kg/m2), and 7 (20.6%) were overweight (BMI 25-30 kg/m2). The most common presenting symptom was hearing disturbance (70.3%), followed by otorrhea (51.4%). Empty sella was noted on computed tomography or magnetic resonance imaging in 15 patients (45.5%). Eight of the 34 patients (23.5%) were found to have superior semicircular canal dehiscence (SCD). Hearing improved with surgical intervention in 25 of 26 patients with hearing loss as a presenting symptom (96%). CSF resolved in 18 of 19 cases (95%). Seventy-three percent of patients reported at least minimal improvement in vertigo.
TBD may present with symptoms of CSF leak/encephalocele, but may also present with superior SCD. We recommend consistent review of the temporal bone imaging to check for superior SCD, and repair of the SCD first to prevent complications involving the labyrinth and cochlea. MCF approach using a multilayer repair without a lumbar drain is highly effective with minimal risk of complications 1).
2015
Fifty-one patients, 22 males and 29 females, were included in the analysis. The mean age was 48.7 ± 15.5 years, mean body mass index was 32.65 ± 6.86 kg/m(2), and mean symptom duration was 33 ± 42 months. Seven patients underwent repeat surgery for symptomatic recurrence; therefore, there were 58 surgical encounters. Repair included bony reconstruction with hydroxyapatite with or without resection of encephaloceles and/or repair of a dural opening.
According to the MFFD classification system described, 15, 8, 27, and 8 cases were categorized as Class A, B, C, and D, respectively. The prevalence of hearing loss was 87%, 63%, and 70% in Classes A, B, and C, respectively. Vestibular symptoms were more prevalent in Class A. Seven patients reported persistent symptoms at the last follow-up. Transient complications were similar in each classification (13%-25%), and a single permanent complication related to anesthesia was observed. There were no mortalities or severe neurological morbidities in the series.
Middle fossa floor dehiscence has a spectrum of clinical presentations. A classification system may help to clarify the diagnosis and guide therapy. Surgery, the mainstay of treatment, is safe and well tolerated 2)