Intracranial vertebral artery aneurysm
They include aneurysms at the origin of the posterior inferior cerebellar artery (PICA-VA) and aneurysms at the junction of the vertebral and basilar arteries (VA-BA).
Epidemiology
Aneurysms of the vertebral artery are rare, comprising less than 5 percent of all intracranial aneurysms. They can present with subarachnoid hemorrhage, spinal cord compression, and cranial neuropathy.
Vertebral artery (VA) aneurysms in the paediatric population are a rare but a serious condition. However, the epidemiology of paediatric VA aneurysms is poorly understood and there is little consensus on what constitutes the appropriate treatment 1).
In a review of 9709 patients with intracranial aneurysms, 190 with aneurysms at the VA or VA-posterior inferior cerebellar artery junction.
The 190 patients had 193 VA aneurysms, among which 131 (68%) were ruptured. The VA aneurysm caused a mass effect in 7 and ischemia in 2 patients. Compared to 4387 patients with a ruptured aneurysm in other locations, those with a VA aneurysm were older, their aneurysms were more often fusiform, and more often caused intraventricular hemorrhages 2).
Treatment
Videos
Clip reconstruction of giant vertebral artery aneurysm after failed flow reduction therapy
<html><iframe width=“560” height=“315” src=“https://www.youtube.com/embed/-AUVk6nxefQ” frameborder=“0” allowfullscreen></iframe></html>
Outcome
Vertebral artery aneurysms form a group of aneurysms having high rates of rebleeding, morbidity, and mortality, poor treatment outcomes, as well as low rate of surgical treatment 3).
Case series
2015
Lehto et al. reviewed retrospectively 9709 patients with intracranial aneurysms. Of these, they included 190 with aneurysms at the VA or VA-posterior inferior cerebellar artery junction. These patients were treated in the Department of Neurosurgery, Helsinki, Finland, between 1934 and 2011.
The 190 patients had 193 VA aneurysms, among which 131 (68%) were ruptured. The VA aneurysm caused a mass effect in 7 and ischemia in 2 patients. Compared to 4387 patients with a ruptured aneurysm in other locations, those with a VA aneurysm were older, their aneurysms were more often fusiform, and more often caused intraventricular hemorrhages. Among surgically treated aneurysms, clipping was the treatment in 91 (88%) saccular and 11 (50%) fusiform aneurysms. Treatment was endovascular in 13 (9%), and multimodal in 6 (4%) aneurysms. Within a year after aneurysm diagnosis, 53 (28%) patients died. Among the survivors, 104 (93%) returned to an independent or to their previous state of life; only 2 (2%) were unable to return home.
Microsurgery is a feasible treatment for VA aneurysms, although cranial nerve deficits are more common than in endovascular surgery. Despite the challenge of an often severe hemorrhage, of challenging morphology, and risk for laryngeal palsy, most patients surviving the initial stage return normal 4).
1990
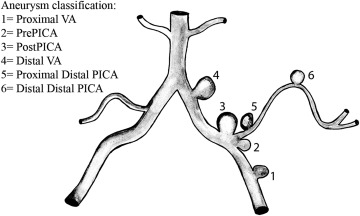
Aneurysms of the posterior inferior cerebellar artery-vertebral artery complex are relatively uncommon lesions. They include aneurysms at the origin of the posterior inferior cerebellar artery (PICA-VA), aneurysms on the distal artery (PICA) and aneurysms at the junction of the vertebral and basilar arteries (VA-BA). We have had the opportunity to treat 17 patients and study the radiological records of 9 additional patients in the past 8 years. The aneurysms ranged in size from 3 to 30 mm, with mean values of 10.6, 7.3, and 9 mm for PICA-VA lesions, distal PICA lesions, and VA-BA lesions, respectively. Three of the 4 VA-BA aneurysms were located at the midline, and the mean distance of the PICA-VA aneurysms from the midline was 7.6 to 9.4 mm; 2 aneurysms crossed the midline from their parent VA. The aneurysms were located slightly more often on the left side (left:right ratio, 1:2), were found more frequently in women (2.25:1), and occurred at a mean age of 50 years. Ten aneurysms at the origin of the PICA and 4 VA-BA aneurysms were treated via a lateral suboccipital craniectomy; 3 distal PICA aneurysms were exposed by a midline craniectomy. Surgery was carried out acutely in 5 patients. Tortuousness of the VA required contralateral approaches in 2 patients, an exploratory craniectomy in 1 patient, and an approach toward the dome of 1 patient with a VA-BA aneurysm. Morbidity was primarily due to cranial nerve dysfunction. There were no perioperative deaths. These aneurysms can easily be missed on initial radiographic examination; one appeared only on the second study, one was seen to grow over 16 days, and one was discovered at the level of C1 extracranially. Our radiographic and surgical approach to the treatment of these lesions is presented 5).
Case reports
An extremely rare case of a small ruptured aneurysm of the leptomeningeal collateral circulation from the vertebral artery (VA) to the posterior inferior cerebellar artery (PICA); this aneurysm was associated with bilateral VA occlusion. A 72-year-old woman with sudden headache, nausea, and subarachnoid hemorrhage (SAH) was admitted to our hospital. On admission, no evidence of cerebral signs or cranial nerve palsy was found. Computed tomography imaging showed SAH predominantly in the posterior fossa, and digital subtraction angiography revealed bilateral VA occlusion and the left VA aneurysm located proximal to the VA union. In addition, a small aneurysm was observed at the leptomeningeal collateral circulation located between the extracranial left VA and the left PICA. The patient underwent radical surgery on the day of the onset of the symptoms associated with SAH. However, the VA aneurysm was unruptured and surgically trapped. The small aneurysm arising at the leptomeningeal collateral circulation was ruptured during the surgery and was electrocoagulated; the collateral circulation was preserved, and no neurologic deficits were observed. The postoperative course was uneventful. SAH with the occlusion of major vessels should be diagnosed with utmost caution to allow preoperative neurologic and radiological assessments 6).
A 68-year-old Caucasian man with occlusion of the right vertebral artery and a ruptured aneurysm at the junction of the left posterior inferior cerebellar artery-left vertebral artery that was successfully treated by the deployment of a single flow-diverting stent in the stenotic left vertebral artery. Stent deployment was complicated by thrombotic occlusion of the basilar artery, which was successfully reopened. The patient recovered completely, and follow-up angiography at 4 months and 1 year showed patent vertebral artery with gradual shrinkage of the aneurysm.
This report contributes to the literature on treatment of large ruptured aneurysms localized in stenotic arteries and in areas of the endocranium where a mass of embolic material in the aneurysm (coils) might compromise the circulation in the parent blood vessel or compress vital brain structures 7).
Examinations for subarachnoid bleeding revealed a vertebral artery aneurysm with a diameter of 12 mm in a 67-year-old man who presented with headache. The vertebral artery aneurysm with saccular and fusiform segments was shrunk and clipped via lateral left suboccipital approach. No neurologic deficit was present at the postoperative period. Control digital subtraction angiography showed complete shrinkage of aneurysm with continued blood flow and no residue. Clinical findings, treatments, and surgical approaches of VA aneurysms are different from anterior and posterior circulation aneurysms. Microneurosurgical clipping is the most effective treatment of vertebral artery aneurysms in suitable cases. Although endovascular intervention is commonly applied as therapeutic modality for patients with vertebral artery aneurysm, researchers have also emphasized that saccular vertebral aneurysms with fusiform extension can also be surgically treated in suitable cases 8).