Convexity meningioma diagnosis
see also Magnetic resonance imaging for intracranial meningioma diagnosis.
Meningiomas are most commonly discovered incidentally before a patient experiences any symptoms. The most common way a convexity meningioma is diagnosed is when a magnetic resonance imaging (MRI) or computed tomography (CT) scan is performed following an accident or when a patient presents with symptoms unrelated to the growth such as headache, hearing loss, dizziness, and vertigo, among other neurological deficits. The tumor will appear on the scan.
There is a need for prompt neuroimaging of the brain when patients present any atypical psychiatric symptoms, with late-onset (> 50 years old) of the first depressive episode or fast changes of the mental state 1).
In most situations MRI gives all the information one needs.
Preoperative radiologic classification
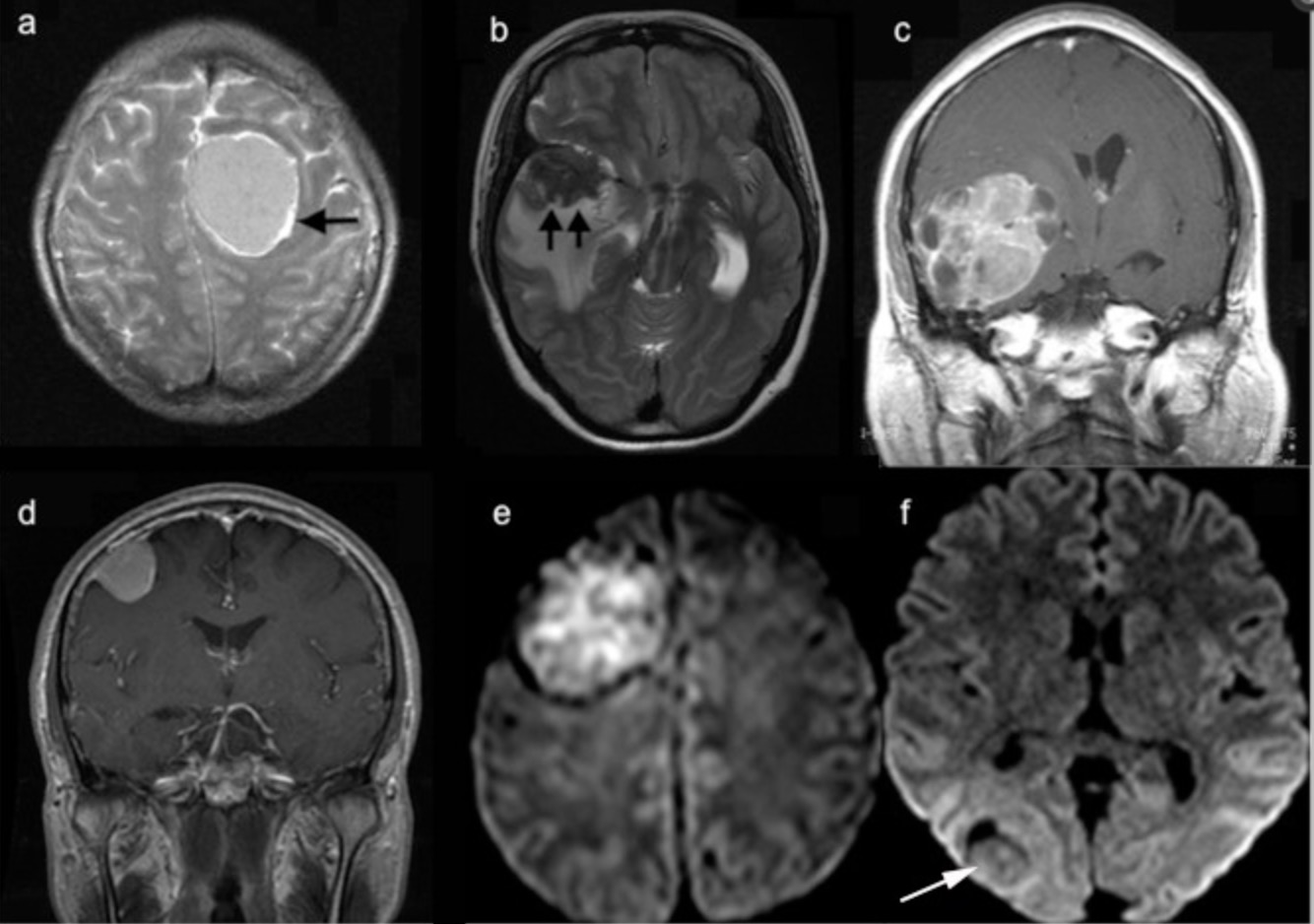
Preoperative radiologic parameters were analyzed, each parameter was scored 0 or 1. Signal intensity on diffusion weighted MRI (DWI) (hyperintensity=1), heterogeneity on T1-weighted gadolinium enhanced MRI (heterogeneity=1), disruption of arachnoid at brain-tumor interface=1and peritumoral edema (PTE) on T2-weighted MRI (presence of PTE=1) and tumor shape (irregular shape=1). Multivariate logistic regression analyses were conducted to determine association of radiological parameters to histopathological grading. Kaplan-Meier and Cox regression models were used to determine the association of scoring system to overall survival and progression free survival (PFS). Reliability of the classification was tested using Kappa co-efficient analysis.
Hyperintensity on DWI, disruption of arachnoid at brain-tumor interface, PTE, heterogenicitiy on T1-weighted enhanced MRI and irregular tumor shape were independent predictors of non-grade I meningioma. Mean follow-up period was 94.6 months (range, 12-117 months). Median survival and PFS in groups-I, II and III was 114.1±1.2 and 115.7± 0.8, 88± 3.3 and 58.5±3.9, 43.2± 5.1 and 18.2±1.7 months respectively. In cox regression analysis model, age (P<0.0001, OR-1.039, CI-1.017-0.062), WHO non-grade-I meningioma (P=0.017, OR-3.014, CI-1.217-7.465), radiological classification groups II (P=0.002, OR-6.194, CI-1.956-19.610) and III (P<0.0001, OR-21.658, CI-5.701-82.273) were independent predictors of unfavorable survival outcomes.
Preoperative radiological classification can be used as a supplement to the histopathological grading. Group-I meningiomas demonstrate benign radiological, histopathological and clinical features; group-III demonstrates aggressive features. Group-II meningiomas demonstrate intermediate features; the need for more aggressive follow-up and/or treatment should be further investigated 2).
a) T2-weighted MRI demonstrating the complete arachnoid ring (black arrow) and no peritumoral edema; b) T2-weighted MRI demonstrating the disappearance of arachnoid ring (black arrow head) and peritumoral edema c) T1-weighted gadolinium enhanced MRI demonstrating heterogeneous enhancement and irregular shape of the tumor; d) T1-weighted gadolinium enhanced MRI demonstrating homogenous enhancement and regular shape of tumor; e) Diffusion weighted MRI demonstrating hyperintense lesion; f) Diffusion weighted MRI demonstrating isointense lesion.