Cerebral aqueduct
The cerebral aqueduct, also known as the aqueductus mesencephali, mesencephalic duct, or the aqueduct of Sylvius is within the mesencephalon (or midbrain), contains cerebrospinal fluid (CSF), and connects the third ventricle in the diencephalon to the fourth ventricle within the region of the mesencephalon and metencephalon, located dorsal to the pons and ventral to the cerebellum.
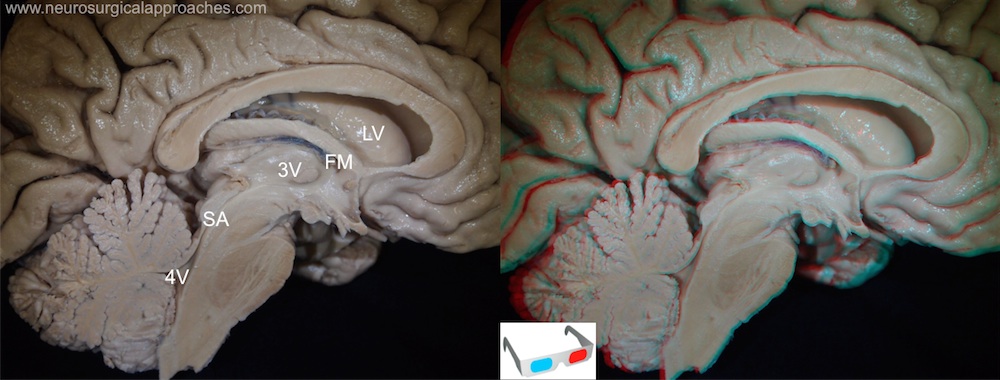
SA: Aqueduct of Sylvius
The aqueduct of Sylvius is the channel which connects the third ventricle to the fourth ventricle and is the narrowest part of the CSF pathway with a mean cross-sectional area of 0.5 mm2 in children and 0.8 mm2 in adults.
see Aqueductal tumor.
MR imaging has been proposed to quantify the flow of CSF in the aqueduct.
By phase contrast magnetic resonance imaging (PCCMR), the stroke volume (SV), defined as the mean volume passing through the aqueduct during both systole and diastole, can be calculated. A SV greater than or equal to 42 μL serves as a selection criterion for patients with good probabilities of improvement after VPS.
Prospective observational studies with a technical development focus
No dedicated platform exists for quantifying pressure differences across the aqueduct (ΔP), and no research has been conducted on the impact of breathing on ΔP. A study aims to develop a post-processing platform that balances accuracy and ease of use to quantify cerebral aqueduct resistance and, in combination with real-time phase contrast MRI, quantify ΔP driven by free breathing and cardiac activities.
Thirty-four healthy participants underwent 3D balanced fast field echo (BFFE) sequence and real-time phase contrast (RT-PC) imaging on a 3T scanner. Liu et al. used the developed post-processing platform to analyze the BFFE images to quantify the aqueduct morphological parameters such as resistance. RT-PC data were then processed to quantify peak flow rates driven by cardiac and free breathing activity (Qc and Qb) in both directions. By multiplying this Q by resistance, ΔP driven by cardiac and breathing activity was obtained (ΔPc and ΔPb). The relationships between aqueduct resistance and flow rates and ΔP driven by cardiac and breathing activity were analyzed, including a sex difference analysis.
The aqueduct resistance was 78 ± 51 mPa·s/mm³. The peak-to-peak cardiac-driven ΔP (Sum of ΔPc+ and ΔPc-) was 24.2 ± 11.4 Pa, i.e., 0.18 ± 0.09 mmHg. The peak-to-peak breath-driven ΔP was 19 ± 14.4 Pa, i.e., 0.14 ± 0.11 mmHg. Males had a longer aqueduct than females (17.9 ± 3.1 mm vs. 15 ± 2.5 mm, p < 0.01) and a larger average diameter (2.0 ± 0.2 mm vs. 1.8 ± 0.3 mm, p = 0.024), but there was no gender difference in resistance values (p = 0.25). Aqueduct resistance was negatively correlated with stroke volume and the peak cardiac-driven flow (p < 0.05); however, there was no correlation between aqueduct resistance and breath-driven peak flow rate.
The highly automated post-processing software developed in this study effectively balances ease of use and accuracy for quantifying aqueduct resistance, providing technical support for future research on cerebral circulation physiology and exploring new clinical diagnostic methods. By integrating real-time phase contrast MRI, this study is the first to quantify the aqueduct pressure difference under the influence of free breathing. This provides an important physiological reference for further studies on the impact of breathing on transmantle pressure and cerebral circulation mechanisms 1)
While the findings are promising, they are preliminary, and further studies with larger sample sizes, disease populations, and longer follow-up periods are needed to validate these results and explore their clinical implications. The lack of a detailed description of the software’s algorithms and technical specifications also limits the broader applicability of the approach, and future papers should provide more transparency in this area to ensure reproducibility and robustness. Nevertheless, this research opens the door to a better understanding CSF circulation and its potential role in neurodegenerative diseases.