Table of Contents
Traumatic brain injury CT Classification
Key Parameters
The classification considers the following CT findings:
- Traumatic Subarachnoid Hemorrhage (tSAH):
- Presence or absence is noted.
- Extent of hemorrhage contributes to overall grading.
- Epidural Hematoma (EDH):
- Evaluated for size and mass effect.
- Subdural Hematoma (SDH):
- Thickness and associated midline shift are considered.
- Basal Cisterns:
- Classified as open, compressed, or obliterated.
- Obliteration suggests severe brain swelling and higher mortality risk.
- Midline Shift:
- No shift, <5 mm, or ≥5 mm.
- Indicates the degree of mass effect caused by hemorrhages or swelling.
- Diffuse Axonal Injury (DAI):
- Presence of small hemorrhages in characteristic locations (corpus callosum, brainstem).
Grading and Prognosis
The Stockholm CT Classification groups findings to predict outcomes:
- Mild TBI: Normal CT findings or minimal localized hemorrhages (e.g., isolated tSAH without mass effect).
- Moderate TBI: Moderate hemorrhages (e.g., SDH or EDH) with mild midline shift or basal cistern compression.
- Severe TBI: Extensive hemorrhages, significant midline shift (≥5 mm), or obliterated basal cisterns.
Higher severity grades correlate with increased mortality and poorer functional outcomes.
Clinical Use
- Triage and Decision-Making: Determines the need for interventions such as ICP monitoring, surgical evacuation, or intensive care management.
- Prognostic Tool: Guides discussions with families about expected recovery and outcomes.
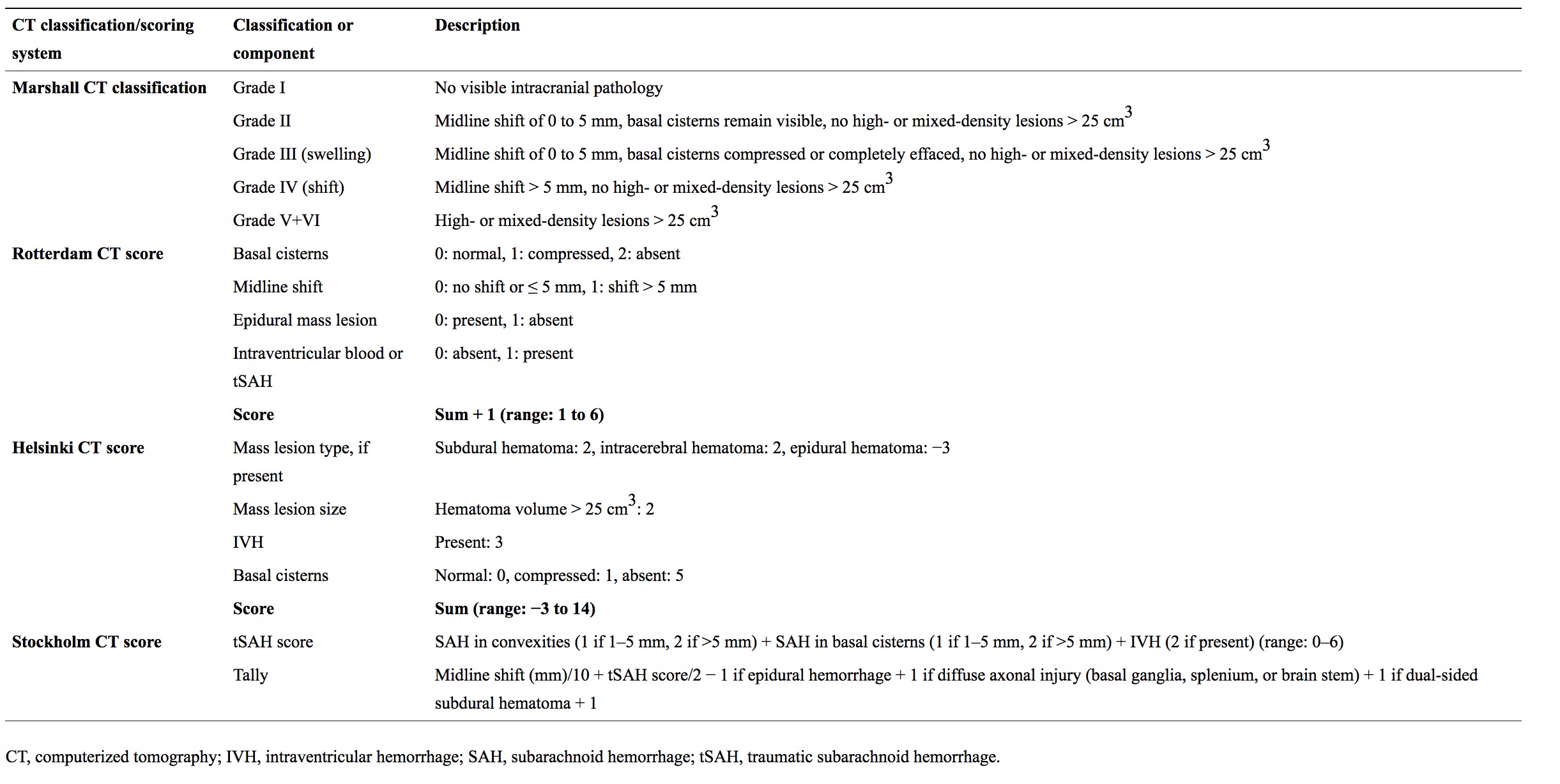
Comparison with Other Classifications
| Feature | Stockholm CT Classification | Helsinki CT Score | Rotterdam CT Score | Marshall CT Classification |
| ————————– | ———————————– | ——————————- | ——————————— | ——————————— |
| Focus | Comprehensive imaging-based TBI stratification. | Focuses on detailed lesion scoring. | Emphasizes prognosis using CT findings. | Broad categorization of injury severity. |
| Incorporates tSAH | Yes, explicitly. | Yes, explicitly. | Yes, explicitly. | Implicitly included. |
| Parameters | tSAH, EDH, SDH, cisterns, midline shift, DAI. | tSAH, SDH, EDH, ICH, cisterns, midline shift, DAI. | tSAH, basal cistern compression, midline shift, hematomas. | Brain swelling, mass lesions, midline shift. |
| Ease of Use | Moderate—requires assessment of multiple features. | Moderate—detailed scoring. | Moderate—simpler than Helsinki. | Easy—broad categories. |
Example Case
Case Details: A 50-year-old male presents with moderate TBI after a fall. CT findings:
- tSAH in the left sylvian fissure.
- SDH measuring 12 mm with a midline shift of 6 mm.
- Obliterated basal cisterns.
- No evidence of DAI.
Classification: Severe TBI - Significant mass effect (midline shift ≥5 mm) and basal cistern obliteration suggest a poor prognosis.
Clinical Relevance
The Stockholm CT Classification ensures all critical CT findings are considered systematically. While not as widely used as the Marshall or Rotterdam systems, it provides a valuable tool in research and specific clinical settings.
Currently, several types of CT classification systems exist to prognosticate and stratify TBI patients. Introduced in 1991, the Marshall computed tomography classification 1) categorizes injuries as different levels of diffuse lesions, based on basal cistern compression and midline shift, or focal lesions, depending on whether lesion volume exceeds 25 cm3. Despite somewhat arbitrarily chosen cutoffs, this classification is still considered to be somewhat of a “gold standard” for TBI classification. While components of the Marshall computed tomography classification have been shown to contribute to outcome prediction in TBI 2), the Marshall computed tomography classification was not originally designed as a prognostic tool. Thus, in 2005, the Rotterdam CT score was introduced, reweighting components of the Marshall computed tomography classification and adding traumatic subarachnoid hemorrhage (tSAH) and intraventricular hemorrhage 3) , creating an ordinal score. Components from the Rotterdam CT score are today an integral part of the International Mission for Prognosis and Analysis of Clinical Trials in TBI (IMPACT) outcome model for TBI patients 4).
More recently, new CT classifications have emerged, including the Stockholm CT score in 2010 5) and the Helsinki CT score in 2014 6). The Stockholm CT score uses midline shift as a continuous variable (as compared to the Marshall computed tomography classification’s and Rotterdam CT score’s threshold of ≥5 mm) and has a separate scoring for tSAH 7). It is also the only scoring system that takes diffuse axonal injury (DAI) visible on CT into consideration 8). Moreover, the Stockholm CT score remains the only scoring system that is based on many features of CT scans examined prospectively using an extended protocol, to identify information content. The Helsinki CT score is based on components from both the Marshall computed tomography classification and Rotterdam CT score, but additionally focuses more on the types of intracranial injuries present 9). Thus, the Stockholm and Helsinki CT scoring systems more comprehensively analyze different components of the admission CT scan, and have both been shown to be better outcome predictors than the Marshall computed tomography classification and Rotterdam CT score 10) 11).
The Stockholm and Helsinki CT scores provide more information on the damage sustained, and give a more accurate outcome prediction, than earlier classification systems. The strong independent predictive value of tSAH may reflect an underrated component of TBI pathophysiology. A change to these newer CT scoring systems may be warranted 12).
Marshall head computed tomography (CT) classification for traumatic brain injury is widely used as a predictor of outcome. However, this grading system lacks the following variables, which are found to be useful predictors: subarachnoid/intraventricular hemorrhage, extradural hematoma, and extent of basal cistern compression. A new classification called the Rotterdam CT score, incorporating the above variables, was proposed later.
Both Marshall and Rotterdam CT score are good in predicting early mortality after moderate and severe TBI 13).
As the Rotterdam system also includes additional variables like subarachnoid hemorrhage, it may be preferable, particularly in patients with diffuse injury 14).
Use of the novel Helsinki CT score improved outcome prediction accuracy, and the Helsinki CT score is a feasible alternative to the Rotterdam and Marshall CT systems. External validation of the Helsinki CT score is advocated to show generalizability 15).