Table of Contents
Transsylvian approach
see also Transsylvian transinsular approach.
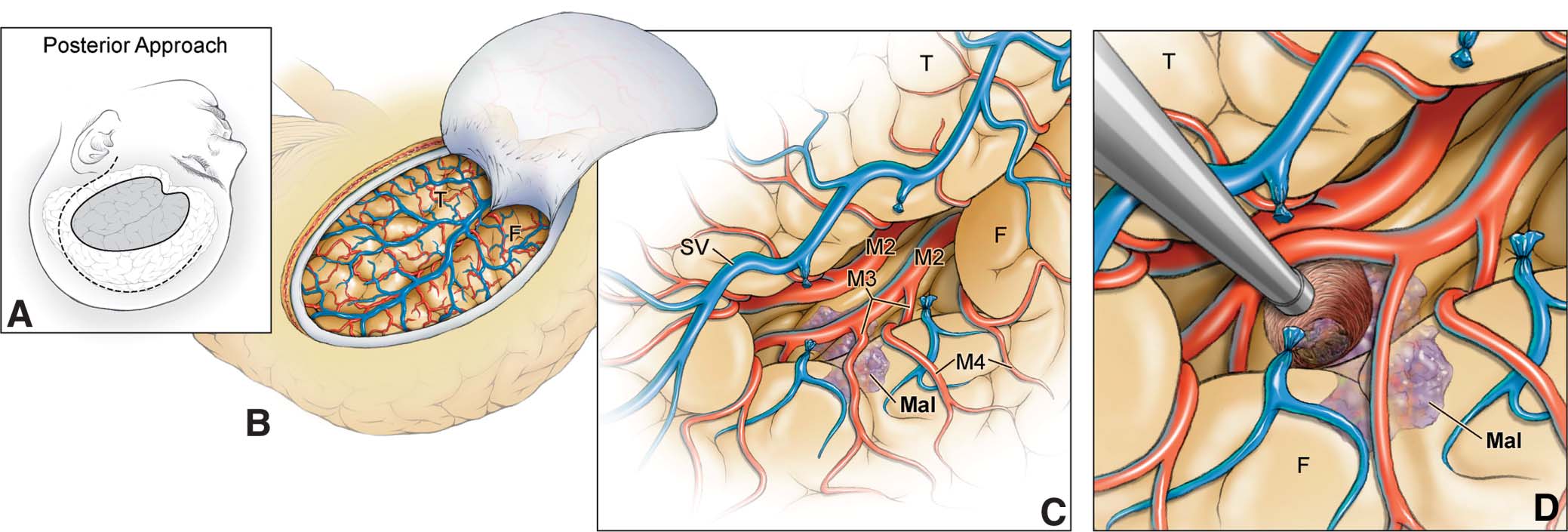
The anterior approach opened the sphenoidal and insular portions of the sylvian fissure and exposed the limen insulae and short gyri of insula, whereas the posterior approach opened the insular and opercular portions of the sylvian fissure and exposed the circular sulcus and long gyri.
see also Transtemporal transchoroidal fissure approach
The transsylvian approach 1) through a pterional craniotomy 2) 3) is particularly useful for anterior basal extrinsic lesions and for frontobasal, mesial temporal, and insular intrinsic intracranial lesions.
Transsylvian-transinsular approaches safely expose vascular pathology in or deep to the insula while preserving overlying eloquent cortex in the frontal and temporal lobes. The anterior transsylvian-transinsular approach can be differentiated from the posterior approach based on technical differences in splitting the sylvian fissure and anatomic differences in final exposure. Discriminating patient selection and careful microsurgical technique are essential 4).
A transsylvian anteromedial approach through the pyriform cortex at the level of the anterior and superior surface of the uncus enables a safe entry into the temporal horn without injury to the optic radiation fibers or the main part of the uncinate fasciculus 5).
Indications
see Transsylvian approach to middle cerebral artery aneurysm.
A study aimed to improve the accuracy and efficacy of the keyhole transsylvian approach to remove hypertensive basal ganglia hemorrhage. Lin et al. presented a stable keyhole craniotomy based on anterior squamosal suture to expose insular cortex and basal ganglia.
Twenty-nine patients with hypertensive basal ganglia hemorrhage were treated with keyhole surgery and studied in Guangdong sanjiu brain hospital.
By using a bone suture marked keyhole transsylvian approach, near-complete (90%) hematoma evacuation was achieved in 21 cases (72.4), 70% to 90% in 8 cases (24.1), and less than 70% in 1 case (3.4%). In our cohort, 55.1% (16/29) with good function (GOS score 4-5), 41.3% (12/29) with disability (GOS score 3), and 3.4% (1/29) in a vegetative state (GOS score 2). No patients died within 6 months of operation.
This method can greatly minimize the bone exposure and precisely located the distal Sylvian fissure. A stable keyhole craniotomy based on bone suture can be identically safe and effective in comparison with classic surgery, and it consumes less time and less intra-operative bleeding 6).
Complications
Ischemic injury as a result of damage to the lenticulostriate artery or MCA branches is one of the main causes of surgical morbidity associated with insular tumor resection. To avoid these complications, a thorough knowledge of the regional anatomy, meticulous microsurgical technique, hemostasis, and gentle handling of the vasculature are crucial.
The transsylvian approach requires to be comfortable with microsurgical techniques to dissect the sylvian fissure. Insular tumors often extend into the white matter covered by frontal and temporal opercula. Initial transsylvian resection and subsequent extension of the opercular operative corridor allows for comfortable access to the insula and subsequent subpial resection with protection of the vasculature. In tumors limited to the insular lobe, Rey-Dios and Cohen-Gadol have routinely used the transsylvian approach without any significant complication. Injury to the descending motor fibers can be another source of morbidity and should be avoided with careful identification of distal LLAs more anteriorly and subcortical mapping at the level of the internal capsule more posteriorly along the resection cavity. The long M2 perforating arteries leading to the corona radiata and central lobule should be also preserved on the surface of the insula and not coagulated inadvertently in case of excessive bleeding from the tumor. Another common cause of morbidity after the transsylvian approach is excessive retraction on the opercular areas, which can result in damage to the Broca area, the horizontal fibers of the arcuate fasciculus near the superior periinsular sulcus, or the fibers of the uncinate fasciculus near the inferior periinsular sulcus. Damage to any of these structures can result in different degrees of speech disturbance or memory impairment, especially on the dominant side.18 To prevent this type of injury, we discourage the use of fixed retractors, and we encourage the use of a “dynamic retraction” technique, using only the suction and bipolar instruments to apply retraction to different areas while constantly shifting the pressure points.
A thorough understanding of the mapping technique becomes even more critical when limited exposures are performed, and the surgeon must rely on “negative stimulation” without identification of unexposed “positive” eloquent areas 7).