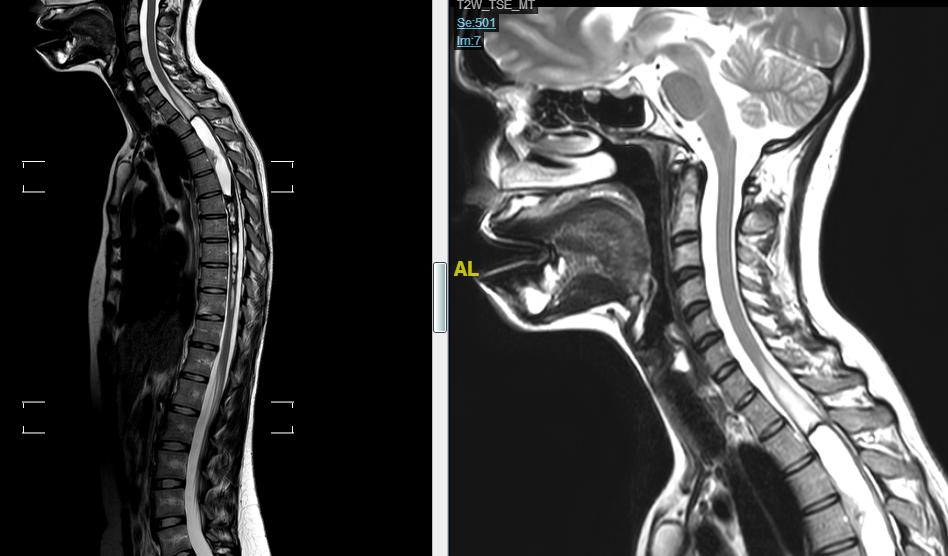
Spinal Ependymoma Magnetic Resonance Imaging
MRI is the modality of choice for evaluating suspected spinal cord tumors.
Features include:
widened spinal cord (as ependymomas arise from ependymal cells lining the central canal, they tend to occupy the central portion of the spinal cord and cause symmetric cord expansion)
although unencapsulated, they are well-circumscribed
tumoral cysts are present in 22%. Non-tumoral cysts are present in 62%.
Syringohydromyelia occurs in 9-50% of cases
In contrast to intracranial ependymomas, calcification is uncommon
average length of four vertebral body segments
Typical signal characteristics:
T1: most are isointense to hypointense; mixed signal lesions are seen if cyst formation, tumour necrosis or haemorrhage has occurred.
T2: hyperintense
peritumoural oedema is seen in 60% of cases
associated haemorrhage leads to the “cap sign” (a hypointense haemosiderin rim on T2 weighed images) in 20-33% of cases.
The cap sign is suggestive of but not pathognomonic for ependymoma as it may also be seen in Spinal cord hemangioblastomas and paragangliomas.
T1 C+ (Gd): virtually all enhance strongly, somewhat inhomogeneously.
Hypointensity at the tumor margin was found to be a relatively firm pseudocapsule, and Hypointensity within the tumor corresponded to intratumoral hematoma. All of the tumors with Hypointensity were ependymomas at histologic examination. When MR imaging shows an intramedullary tumor with Hypointensity at the tumor margin, it is suggestive, but not pathognomonic, of an ependymoma 1).
Intramedullary expansive lesion compatible with neoplasia of about 13.4 cm in length, originating at the level of C4-C5 up to D4-D5, presenting cranial and caudal cystic areas and a solid component at the Th1-Th3 level presenting enhancement of about 43 mm in diameter length and another solid component at the C5 level of 11 mm in length. At the caudal level, the lesion presents a hemosiderin cap or bleeding, slightly hyperintense on T1 and hypointense on T2. Given its location and radiological appearance, it suggests that it is an ependymoma. Extensive spinal cord edema proximal and distal to the lesion is associated, extending from the tectum to T8. Leptomeningeal enhancement along the entire spinal cord and some roots of the cauda equina (more evident in right L5) compatible with tumor extension along the neuraxis. Vertebral lesion affecting the pedicle and the left lamina of Th8 that appears slightly hypointense on T1 and hyperintense on STIR and T2, with contrast enhancement. The lesion appears to present some hypointense septum on T2, it could present some medulla foci inside it, so it probably corresponds to an atypical hemangioma.
On MRI majority of 12(63.2%) of the cord ependymomas and a majority of 5(62.5%) astrocytomas were in the cervical region. While considering axial location ependymomas are mostly 17(89.5%) central and astrocytomas 5(62.5%) are eccentric in location. It was observed that out of 19 cases of ependymoma more than half 10(52.6%) had elongated shapes, and 12(63.1%) had well-defined margins. Associated syringohydromyelia was present in 16(84.2%) cases. On T1WI 11(57.9%) and 8(42.1%) cases were iso and hypo respectively. On T2WI 14(73.7%) cases were hyper-intense. After Gd-DTPA in most cases, 13(68.4%) cases showed diffuse enhancement. Noticeable and sizeable solid components were observed among 13(68.4%) of the cases. Hemorrhage with a cap sign was found in more than one-third of 7(36.8%) cases. Out of 8 cases of astrocytomas 4(50.0%) had lobulated shape, ill-defined margin 5(62.5%). T1WI: Iso 5(62.5%), hypo 3(37.5%), T2WI: hyper 5(62.5%), After Gd-DTPA: focal and heterogenous enhancement 3(37.5%) and rim enhancement 4(50.0%). Component: mixed 4(50.0%), cystic 3(37.5%) and solid 1(12.5%). Hemorrhage without cap sign 2(25.0%), associated syringohydromyelia 1(12.5%). In the case of evaluation of intramedullary ependymoma sensitivity of MRI in the present series is 94.44%, specificity 80.0%, Positive predictive value (PPV) 89.5%, Negative predictive value (NPV) 88.9% and accuracy 89.28%. In the case of MRI evaluation of intramedullary astrocytoma sensitivity of MRI in the present study is 85.71%, specificity 90.47%, PPV 75%, NPV 95%, and accuracy 89.2%. Thus present study shows MRI is a sensitive and effective noninvasive imaging modality in diagnosing common intramedullary spinal cord tumors 2)