Table of Contents
Giant Ophthalmic Artery Aneurysm
Giant Ophthalmic Artery Aneurysm is a giant paraclinoid aneurysm considered a giant aneurysm of the ophthalmic segment of the internal carotid artery.
Abnormalities relating to vision were not identified until the aneurysm realized giant proportions. The optic nerve was typically displaced superomedially, which restricted contralateral extension until late in the clinical course; unilateral nasal field loss was seen in 12 patients. 1).
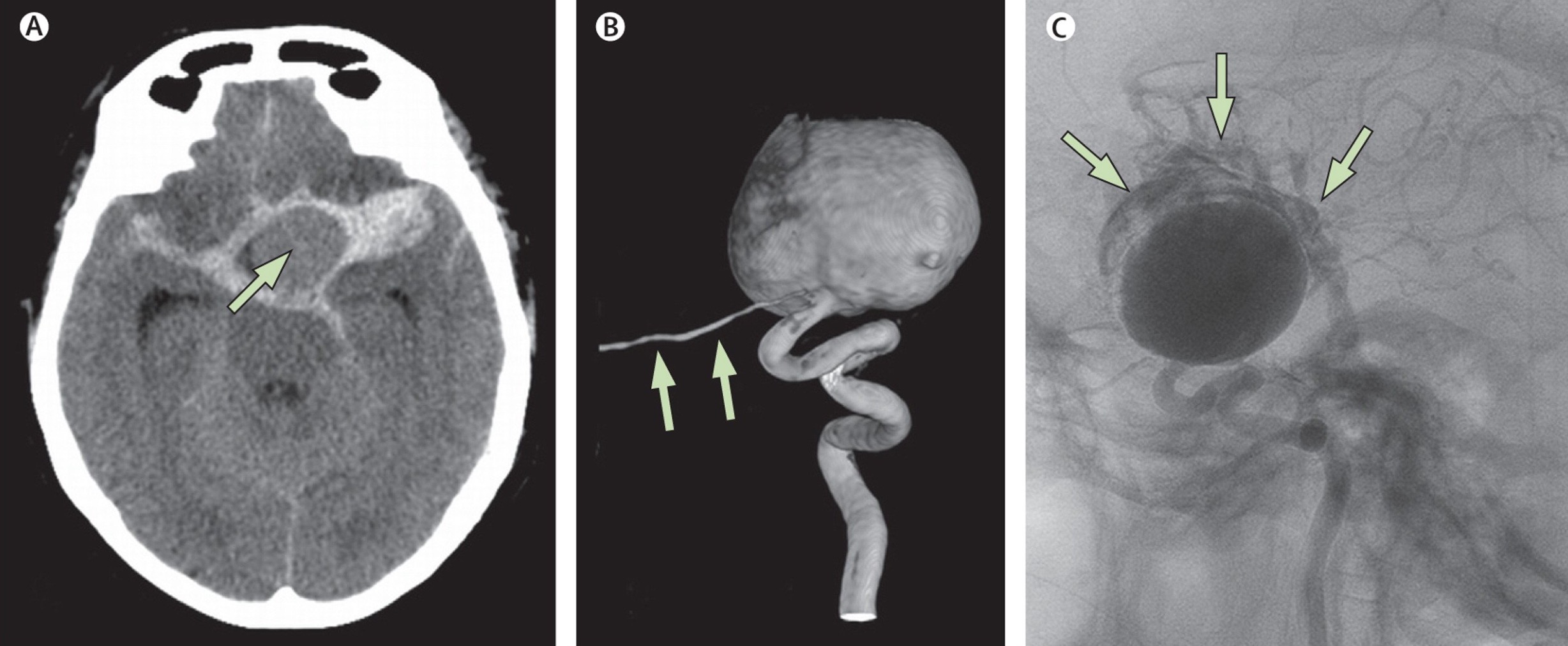
(A) CT of the head shows a subarachnoid haemorrhage from a giant left carotid artery aneurysm (arrow). (B) Three-dimensional impression from the carotid-ophthalmic aneurysm; the ophthalmic artery arises from the sac (arrows). (C) Photograph from rotational run showing extravasation from contrast into the subarachnoid space 2).
In the angiography a notch can often be observed in the anterior superior medial aspect of giant ophthalmic artery aneurysm due to the optic nerve 3).
Treatment
When treating large unruptured ophthalmic artery (OA) aneurysms causing progressive blindness, surgical clipping is still the preferred method because aneurysm sac decompression may relieve optic nerve compression.
There is considerable surgery-related risk for optic pathways during treatment of very large and giant ophthalmic segment aneurysms. Surgery, however, seems to be the treatment of choice in terms of overall visual outcome and aneurysm obliteration 4).
Standard endovascular therapy has shown little success in treatment of very large and giant ophthalmic segment aneurysms.
However, endovascular treatment of OA aneurysms has made important progress with the introduction of stents. Although this development is welcomed, it also makes the choice of treatment strategy less straightforward than in the past, with the potential of missteps.
Case series
2013
A retrospective review of clinical data and treatment summaries was performed for 18 patients with large or giant carotid artery ophthalmic segment aneurysms managed operatively via retrograde suction decompression. Visual outcomes, Glasgow Outcome Scale (GOS) scores, and operative complications were determined. Postoperative angiography was assessed. RESULTS: During a 17-year period, 18 patients underwent surgery performed using retrograde suction decompression. The mean aneurysm size was 26 mm. Three patients presented with subarachnoid hemorrhage. Fourteen of 18 patients presented with visual symptoms. Eleven (79%) of these 14 patients experienced visual improvement and the remaining 3 (21%) experienced worsened vision after surgery. Of 3 patients without visual symptoms and a complete visual examination before and after surgery, 1 had visual worsening postoperatively. One aneurysm required trapping and bypass, and all others could be clipped. Postoperative angiography demonstrated complete occlusion in 9 of 17 clipped aneurysms and neck remnants in the other 8 clipped aneurysms. One (5.5%) of 18 patients experienced a stroke. Eighteen patients had a GOS score of 5 (good outcome), and 1 patient had a GOS score of 4 (moderately disabled). There were no deaths. There was no morbidity related to the second incision or decompression procedure. Prolonged improvement did occur, and even in some cases of visual worsening in 1 eye, the overall vision did improve enough to allow driving. CONCLUSIONS: Retrograde suction decompression greatly facilitates surgical clipping for large and giant aneurysms of the ophthalmic segment. Visual preservation and improvement occur in the majority of these cases and is an important outcome measure. Developing endovascular technology must show equivalence or superiority to surgery for this specific outcome 5).
2012
Of the 257 patients with ophthalmic and paraophthalmic aneurysms, 38 patients had very large or giant aneurysms. Twenty-one underwent surgical treatment; 19 had direct clipping; 1 had trapping, and 1 underwent trapping and bypass. Fifteen patients had unruptured and six had ruptured aneurysms. The mean follow-up period was 88 months. Six (28%) aneurysms had a small residual neck remnant. Of the 12 patients with documented preoperative visual deficit, 9 (75%) improved, 2 (16%) remained stable, and 1 (8%) worsened. Two patients had mild to moderate new visual deficit. Thus, the surgery-related visual complications were 14%. Eighteen patients (86%) had a good or excellent outcome (GOS IV and V). Presentation with prior visual deficit and poor neurological function were predictors of worse visual and clinical outcome, respectively (P = 0.02 and 0.01).
There is considerable surgery-related risk for optic pathways during treatment of very large and giant ophthalmic segment aneurysms. Surgery, however, seems to be the treatment of choice in terms of overall visual outcome and aneurysm obliteration as compared to the current endovascular results in this subset of patients 6).
2008
Six patients who underwent endovascular treatment of paraclinoid aneurysms at our institutions developed delayed postoperative visual decline. Four were treated with combination hydrogel coated coil and bare platinum coils, one with hydrogel-coated coils, and one with bare platinum coils. Three patients presented with some degree of visual impairment caused by their aneurysms. Catheter angiography performed after the visual decline revealed no etiology in any of the cases. Magnetic resonance imaging was performed in all patients and was unremarkable in two. At follow-up, two had improved, three remained unchanged, and one patient died before any follow-up assessment of her vision.
Both acute and delayed visual disturbances can present after the endovascular treatment of carotid artery paraophthalmic aneurysms. Delayed visual deterioration can be observed up to 35 days after embolization. Although the cause is still undefined, it is likely that the more delayed visual deterioration can be attributed to progression of mass effect and/or perianeurysmal inflammatory change. Our case series raises the possibility that this phenomenon may be more likely with HydroCoil (HydroCoil Embolic System; MicroVention, Aliso Viejo, CA). This possibility should be taken into account by neurointerventionists when selecting a coil type to treat large paraophthalmic aneurysms 7).
In giant, large internal carotid ophthalmic artery aneurysms, revised double lumen balloon catheters introduced directly into the cervical carotid arteries were used successfully to perform suction decompression methods. No general heparinization was used during these maneuvers except for continuous intraluminal irrigation of heparin contained saline. Intraoperative multi-directional portable DSA ascertained complete neck clippings and patency of parent vessels. These methods were tried for 8 cases of large, giant IC ophthalmic aneurysms. Among these 5 patients who complained of incomplete visual failures, visual acuity improved in 3 cases. Postoperative transient hemiparesis were seen in two cases which had partially thrombosed, calcified giant aneurysm and the other was due to prolonged proximal ICA occlusion at its cavernous portion. Neither dead nor severely disabled cases were seen, fortunately. Delayed postoperative conventional angiography disclosed complete neck clippings sparing parent arteries except for only one case. This revised direct carotid puncture method is simple and acceptable because of minimal morbidity 8).
1979
Six cases of carotid-ophthalmic aneurysm submitted to direct operation were studied. 1. One out of six cases died postoperatively (mortality rate 16.7%). 2. Exposure of the internal carotid artery at the neck is absolutely necessary for its temporary occlusion. Temporary occlusion of the internal carotid artery at the neck makes the dissection of the aneurysmal neck easier and prevents the aneurysmal rupture during operation. 3. To cope with various complicated handlings, bifrontal carniotomy is recommended. 4. In order to make easy the dissection of the aneurysmal neck, the unroofing of the optic canal as well as the extensive removal of the tip of the anterior clinoid should be performed. 5. From our experience as well as review of the literature, the surgical result of the giant aneurysms is bad. Some new therapy is expected to be developed for the giant aneurysm of this site 9).
Case reports
2015
Aneurysm Transection and Intra-aneurysmal Clipping of a Giant Ophthalmic Artery Aneurysm: 3-Dimensional Operative Video 10).
2014
A 56-year-old woman presented with a long history of progressive unilateral visual loss and magnetic resonance imaging showing a 20-mm left-sided OA aneurysm. Intervention Because of her long history of very poor visual acuity, we considered her left eye to be irredeemable and opted for endovascular therapy. The OA aneurysms was treated with stent and coils but continued to grow, threatening the contralateral eye. Because she failed internal carotid artery (ICA) balloon test occlusion, we performed a high-flow extracranial-intracranial bypass with proximal ICA occlusion in the neck. However, aneurysm growth continued due to persistent circulation through reversed blood flow in distal ICA down to the OA and the cavernous portion of the ICA. Due to progressive loss of her right eye vision, we surgically occluded the ICA proximal to the posterior communicating artery and excised the coiled, now giant, OA aneurysm. This improved her right eye vision, but her left eye was permanently blind.
This case report illustrates complications of the endovascular and surgical treatment of a large unruptured OA aneurysm 11).
A patient with a giant paraclinoid aneurysm resulting in bilateral visual loss that worsened following placement of a Pipeline Embolization Device and adjunctive coiling. Visual worsening occurred in conjunction with aneurysm thrombosis, increase in maximal aneurysm diameter and new adjacent edema. Her visual function spontaneously improved in a delayed fashion to better than pre-procedure, in conjunction with reduced aneurysmal mass effect, size and pulsation artifact on MRI. This report documents detailed ophthalmologic and MRI evidence for the role of thrombosis, aneurysm mass effect and aneurysm pulsation as causative etiologies for both cranial nerve dysfunction and delayed resolution following flow diversion treatment of large cerebral aneurysms 12).
2013
Visual vignette. Giant partially thrombosed left ophthalmic artery aneurysm 13).
“Successful” coiling of a giant ophthalmic aneurysm resulting in blindness: case report and critical review 14).
A 71-year-old female patient was referred suffering from subarachnoid hemorrhage due to a ruptured giant aneurysm of the ophthalmic segment of the right internal carotid artery (ICA). During the endovascular procedure, a coil migrated in the ICA. Coil dislocation could be treated by either retrieval or fixation. On intention to treat we retrieved the coil with the self-expanding Solitaire(®) AB stent (Ev3, Irvine, CA, USA). The Solitaire(®) stent is established to perform mechanical thrombectomy for treatment of acute stroke. This report demonstrates the Solitaire(®) stent's potential for safe and effective retrieval of dislocated coils. Other retrieval systems will be discussed 15).
2012
A case report is presented which describes a novel complication of delayed intraparenchymal hemorrhage following deployment of a pipeline embolization device for the treatment of a previously ruptured partially thrombosed ophthalmic segment aneurysm 16).
2011
A unique case is presented in which a patient with multiple intracranial aneurysms was treated using a multimodality approach. After an intracranial-extracranial bypass, the left internal carotid artery ophthalmic aneurysm continued to grow on follow-up angiogram. Thus it was decided to go ahead with coiling of the aneurysm. The coils were delivered through the saphenous vein graft. The patient tolerated the procedure well and there were no procedural complications 17).
Rupture of a giant carotid-ophthalmic aneurysm 18).
A 67-year-old woman with an unclippable giant (33mm) carotid ophthalmic aneurysm. High-flow external carotid artery to middle cerebral artery bypass and proximal cervical internal carotid artery Hunterian ligation achieved complete thrombosis. Subsequent expansion of the thrombosed aneurysm created mass effect with hydrocephalus, leading to marked cognitive and visual decline. Aneurysmal decompression led to improved vision and near-normal neurological function 19).
2010
A patient underwent craniotomy for surgical clip ligation of a giant ophthalmic artery aneurysm without resection of the aneurysm mass; the patient then presented again approximately 4 months later with a first-time seizure. Following a second craniotomy for resection of the aneurysm mass, the aneurysm contents were noted on pathological examination to contain gram-positive rods, and the aneurysm wall was noted to contain inflammatory cells. Although cultures were not obtained, Propionibacterium acnes was detected using polymerase chain reaction. To the best of the authors' knowledge, this case represents the second reported case of an intraaneurysmal abscess and the first reported instance of a presumed secondary infection of a giant intracranial aneurysm remnant following surgical clip ligation 20).
2009
A patient with a symptomatic left giant carotido-ophthalmic aneurysm who initially underwent coil embolization with subtotal obliteration. The patient's symptoms were initially stable, but 1 year later, she presented with a rapidly progressive contralateral visual deficit. Although angiogram showed a stable neck remnant, MR confirmed aneurysm growth and showed a new peripheral hematoma in the wall of the thrombosed aneurysm. Surgical exploration was undertaken, and even after trapping and intra-aneurysmal thrombectomy, constant bleeding was observed from the wall of the thrombosed aneurysm consistent with the vasa vasorum. Bleeding stopped after cauterization and partial resection of the aneurysm dome, and the aneurysm was clipped. The patient's recent visual deficit markedly improved, and the angiogram did not reveal any residue. Giant aneurysms may continue to grow due to a hypertrophic vasa vasorum and subadventitial hemorrhages. Surgery should be considered if complete thrombosis of the aneurysm does not alleviate patient's symptoms 21).
1984
The author describe a patient with bilateral giant aneurysms of the internal carotid artery in the region of the ophthalmic artery. These lesions are very rare and can be mistakenly diagnosed as intracranial tumors on the basis of the clinical presentation and CT findings alone. The correct diagnosis is made via cerebral panangiography and a successful surgical treatment for this pathology is often available 22).
1994
A case of the successful clipping of a giant aneurysm of the ophthalmic segment of the internal carotid artery 23)
1975
The authors describe a patient with bilateral giant aneurysms of the internal carotid artery in the region of the ophthalmic artery. This care illustrates the feasibility of successful intracranial surgical treatment for this unusual combination 24).