Table of Contents
Facet joint violation
Latest PubMed Titles
Definition
Facet joint violation (FJV) occurs when a pedicle screw breaches the facet joint, potentially leading to adjacent segment disease (ASD) and postoperative pain.
Epidemiology
| Factor | Details |
|---|---|
| Overall Incidence (by Technique) | - Freehand: 25%–85% - Fluoroscopic Guidance: 15%–45% - CT Navigation: 10%–30% - Robotic Assistance: 5%–20% |
| Incidence by Spinal Level | - Higher at L4–L5 due to anatomical constraints - Lower at L1–L3 due to better trajectory control |
| Risk Factors | - Freehand technique, straight trajectory, lower surgical experience - Degenerative disease, scoliosis, open surgery |
| Clinical Impact | - Increased risk of Adjacent Segment Disease (ASD), chronic pain, higher revision surgery rates |
| Prevention Strategies | - Preoperative CT planning, intraoperative navigation, optimal screw trajectory (Medial-to-Lateral) |
Classification
Various classification systems are used to assess the severity of facet joint violations in spinal instrumentation. Below are some commonly used classifications:
Babu
Grade 0 Screw not in facet
Grade 1 Screw in lateral facet but not in facet articulation
Grade 2 Penetration of facet articulation by screw
Grade 3 Screw travels within facet articulation
Shah
Shah RR, Mohammed S, Saifuddin A, Taylor BA. Radiologic evaluation of adjacent superior segment facet joint violation following transpedicular instrumentation of the lumbar spine. Spine (Phila Pa 1976). 2003 Feb 1;28(3):272-5. doi: 10.1097/01.BRS.0000042361.93572.74. PMID: 12567030.
Park
A: Grade 0. no facet joint violation; B: Grade 1. Hardware within 1 mm from or abutting the facet joint, without clear joint involvement; C: Grade 2. Pedicle screw clearly within the facet joint; D: Grade 3. Pedicle screw head/ connector/ rod clearly within the facet joint.
Babu, Shah and modified Park grading system are reliable grading systems, and it reported comparable violation rate. The self-reported clinical outcomes of patients with FJV were worse at 2-year follow-up. For clinical application, it is recommended to use 2 or even 3 different grading systems together to evaluate the FJV 1)
Biomechanics
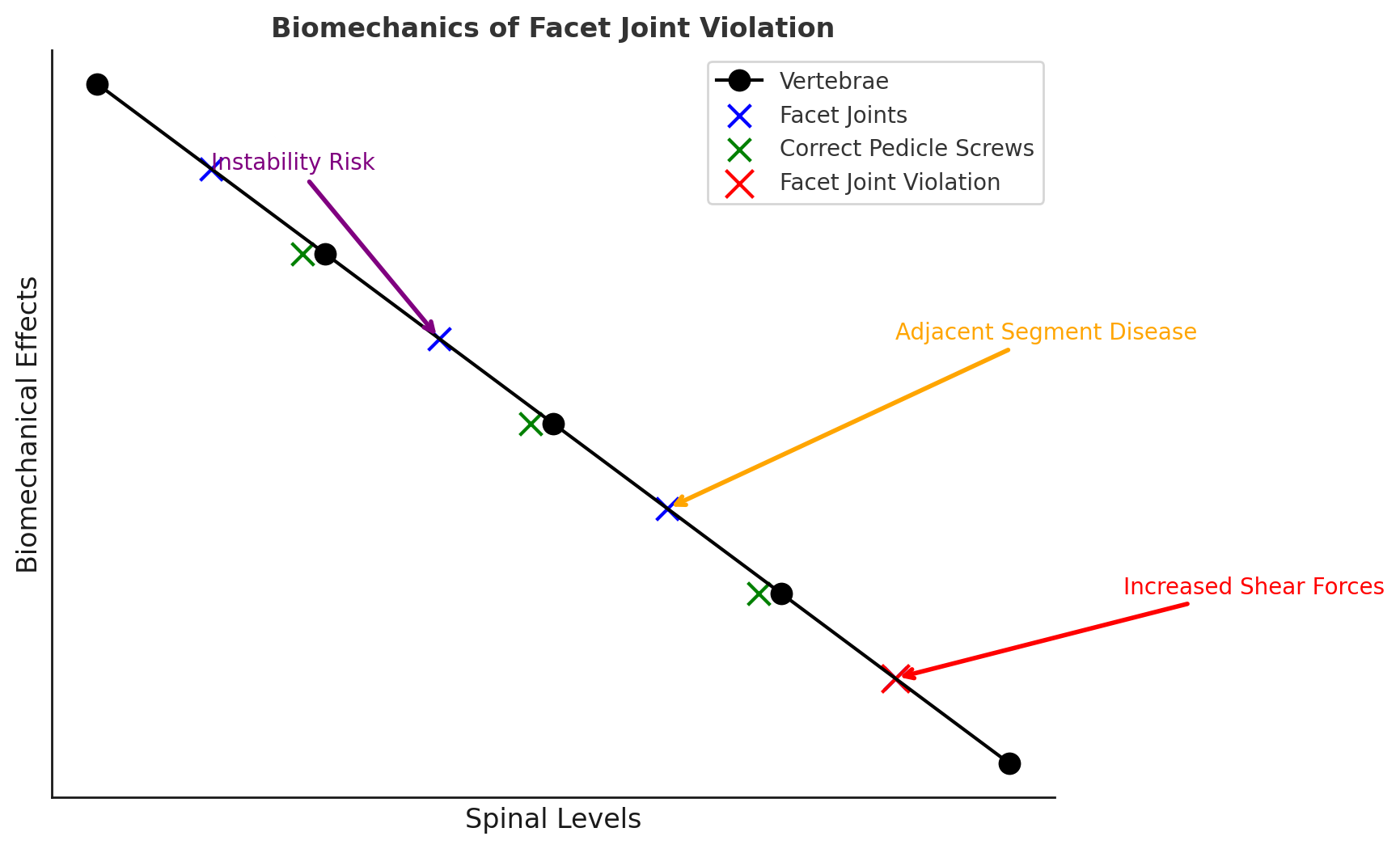
Diagram illustrating the biomechanics of facet joint violation (FJV):
Black circles represent the vertebrae.
Blue dots represent the facet joints, which normally help stabilize the spine.
Green dots represent correctly placed pedicle screws, which avoid facet joint penetration.
The red dot represents a facet joint violation, where a screw has breached the facet joint.
Arrows indicate the biomechanical consequences:
Increased shear forces (red): Leads to instability.
Adjacent segment disease (ASD) (orange): Increased stress on superior levels.
Instability risk (purple): Disrupts spinal mechanics, increasing revision surgery risk.
Clinical features
1. Pain Symptoms Axial Back Pain: Localized pain at the affected spinal level due to mechanical disruption and inflammation. Facetogenic Pain: Referred pain patterns that mimic facet syndrome, radiating to the flank, buttocks, or posterior thighs. Increased Pain with Extension: Pain exacerbation when extending the spine, which loads the facet joints.
2. Neurological Symptoms (Less Common) Radicular Pain: If the facet capsule irritation affects nearby nerve roots. Paresthesias or Weakness: If there is direct nerve compression or irritation.
3. Mechanical Dysfunction Limited Range of Motion: Especially with lumbar extension and lateral bending. Instability Symptoms: If the facet joint is significantly violated, it may contribute to post-surgical instability.
4. Postoperative Findings Early-Onset Postoperative Pain: Patients may experience pain soon after surgery, distinct from typical post-laminectomy discomfort.
Facet Arthritis Acceleration: Violation of the joint may predispose to early degenerative changes.
Facet joint violations are often asymptomatic but can lead to chronic pain, adjacent segment disease, and spinal instability.
Diagnosis
Facet joint violation occurs when surgical instrumentation, such as pedicle screws, breaches the facet joint. Proper diagnosis relies on a combination of clinical evaluation and imaging studies.
1. Clinical Assessment
History & Symptoms
- Persistent or worsening postoperative back pain.
- Pain localized to the affected spinal level.
- Pain aggravated by lumbar extension, lateral bending, or rotation.
- Referred pain to the buttocks or posterior thighs.
- Possible radicular symptoms in severe cases.
Physical Examination
- Palpation: Local tenderness over the affected facet joint.
- Extension-Based Provocation Tests: Pain increases with extension and rotation (Kemp’s test).
- Neurological Exam: Typically normal unless nerve compression is present.
2. Imaging Studies
**CT Scan (Gold Standard)**
- Best modality to confirm facet joint violation.
- Detects pedicle screw misplacement, facet destruction, or osteoarthritis.
- 3D CT reconstructions improve visualization.
**X-Ray (Limited Utility)**
- Standard AP and lateral views: May reveal screw misplacement.
- Oblique views: Can help assess facet joint integrity.
**MRI (Soft Tissue Assessment)**
- Identifies facet joint inflammation or effusion.
- Evaluates nerve root compression if neurological symptoms are present.
**Fluoroscopy (Intraoperative or Diagnostic)**
- Intraoperative fluoroscopy ensures proper screw placement.
- Diagnostic facet joint injection: Pain relief with anesthetic confirms facetogenic pain.
Summary
- CT scan is the gold standard for detecting facet joint violation.
- MRI helps assess inflammation and soft tissue involvement.
- Fluoroscopy and diagnostic injections confirm facet-related pain.
Differential Diagnosis
- Adjacent Segment Disease – Degeneration at adjacent levels mimicking facetogenic pain.
- Failed Back Surgery Syndrome (FBSS) – Persistent pain from multiple potential causes.
- Radiculopathy – Due to direct nerve compression rather than facet involvement.
Prevention
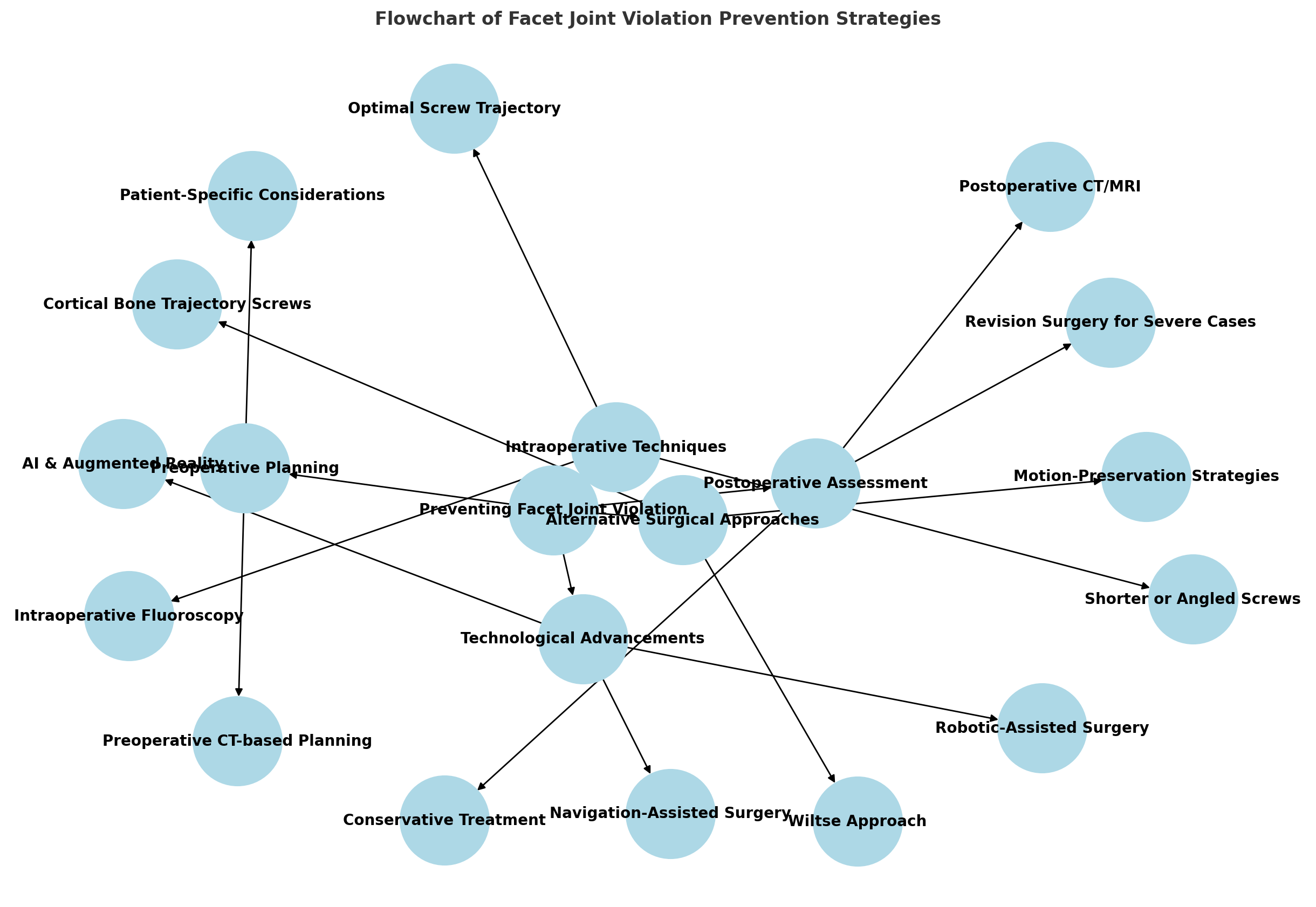
Preoperative Planning:
CT-based planning for precise screw placement. Patient-specific considerations to account for anatomical variability. Intraoperative Techniques:
Optimal screw trajectory (medial-to-lateral) to avoid facet breach. Shorter or angled screws to prevent superior facet impingement. Intraoperative fluoroscopy to confirm screw placement. Technological Advancements:
Navigation-assisted surgery for real-time guidance. Robotic-assisted surgery to optimize screw accuracy. AI & Augmented Reality for improved visualization and planning. Alternative Surgical Approaches:
Cortical Bone Trajectory (CBT) Screws for safer insertion. Wiltse Approach to minimize disruption of midline structures. Motion-preserving strategies to avoid unnecessary fusion. Postoperative Assessment & Management:
CT/MRI scans for early detection. Conservative management for mild violations (physical therapy, NSAIDs). Revision surgery for severe instability or chronic pain.
Treatment
The treatment of facet joint violation depends on the severity of symptoms and the degree of joint involvement. Management strategies range from conservative approaches to surgical revision in severe cases.
1. Conservative Treatment (First-Line)
Patients with mild to moderate symptoms often respond to non-surgical management, including:
**Medications**
- NSAIDs (e.g., ibuprofen, naproxen): Reduce inflammation and pain.
- Muscle relaxants (e.g., baclofen, tizanidine): Address muscle spasm and secondary pain.
- Neuropathic pain agents (e.g., gabapentin, pregabalin): If nerve irritation is present.
**Physical Therapy**
- Postural training: To reduce excessive load on the affected facet joints.
- Core strengthening exercises: Improve spinal stability.
- Manual therapy/mobilization: Relieve facet joint dysfunction and pain.
**Interventional Pain Management**
- Facet Joint Injections (Steroids + Local Anesthetics): Temporary relief and diagnostic value.
- Medial Branch Blocks: If pain relief occurs, it confirms facetogenic pain.
- Radiofrequency Ablation (RFA): Provides longer-term relief by denervating the medial branch nerves.
2. Surgical Treatment (For Severe Cases)
If conservative treatments fail or if facet joint violation leads to instability, surgical options may be necessary.
**Revision Surgery**
- Screw Removal and Repositioning: If misplacement is identified on CT.
- Facet Joint Debridement or Fusion: If joint integrity is compromised.
- Posterior Instrumented Fusion: If instability is present.
**Minimally Invasive Options**
- Endoscopic Facet Joint Debridement: If the joint is inflamed but not severely damaged.
- Percutaneous Rhizotomy: If long-term pain control is needed without major surgery.
3. Prognosis
- Mild violations often improve with conservative care.
- Severe cases with instability may require surgery to prevent long-term complications.
- Early diagnosis and appropriate management improve patient outcomes.
Prospective cohort studies
Studies report the rates of facet joint violation in open procedures to be 24%-100% depending on the specific screw insertion technique utilized 2) 3) 4)
152 patients of lumbar spinal stenosis treated with percutaneous pedicle screw placement were enrolled in a study. facet joint violation (FJV) was evaluated on 3-dimensional lumbar CT reconstruction. Three types of grading systems were used to evaluate FJV: Babu's system (grading by the severity of violation), Shah's system (grading by side of violation), and modified Park's system (grading by different components to cause violation). The violation rate and observer consistency of the 3 grading systems were analyzed. Clinical outcomes were evaluated by visual analog score (VAS), Oswestry disability index (ODI) score.
Kappa coefficients of interobserver consistency on Babu, Shah, and Park grading systems were 0.726,0.849,0.692, respectively. The violation rate of Babu, Shah, and Park grading systems were comparable, which were 34.54%, 32.57%, 33.55%, respectively. In all 3 grading systems, the postoperative VAS low-back pain and ODI scores in non-FJV groups were lower than those in FJV groups (P < .05), and there were no significant differences between 2 groups in VAS leg pain(P >.05).
Babu, Shah and modified Park grading system are reliable grading systems, and it reported comparable violation rate. The self-reported clinical outcomes of patients with FJV were worse at 2-year follow-up. For clinical application, it is recommended to use 2 or even 3 different grading systems together to evaluate the FJV 5) 152 patients of lumbar spinal stenosis treated with percutaneous pedicle screw placement were enrolled in a study. facet joint violation (FJV) was evaluated on 3-dimensional lumbar CT reconstruction. Three types of grading systems were used to evaluate FJV: Babu's system (grading by the severity of violation), Shah's system (grading by side of violation), and modified Park's system (grading by different components to cause violation). The violation rate and observer consistency of the 3 grading systems were analyzed. Clinical outcomes were evaluated by visual analog score (VAS), Oswestry disability index (ODI) score.
Kappa coefficients of interobserver consistency on Babu, Shah, and Park grading systems were 0.726,0.849,0.692, respectively. The violation rate of Babu, Shah, and Park grading systems were comparable, which were 34.54%, 32.57%, 33.55%, respectively. In all 3 grading systems, the postoperative VAS low-back pain and ODI scores in non-FJV groups were lower than those in FJV groups (P < .05), and there were no significant differences between 2 groups in VAS leg pain(P >.05).
Babu, Shah and modified Park grading system are reliable grading systems, and it reported comparable violation rate. The self-reported clinical outcomes of patients with FJV were worse at 2-year follow-up. For clinical application, it is recommended to use 2 or even 3 different grading systems together to evaluate the FJV 6)
Retrospective Matched Cohort Studies
Nilssen et al. investigate and compare the incidence of rostral facet joint violation by pedicle screws under robotic guidance and computerized tomography (CT) navigation guidance.
All patients who underwent robotic-assisted lumbar fusion at a major spine center up until 2023 were retrospectively identified and matched 1:3 to patients undergoing CT navigation guidance based by on age, sex, rostral vertebral level, and length of the construct. Inclusion criteria consisted of age greater than 18 years, bilateral pedicle screw fixation, and the presence of a postoperative CT scan of the lumbar spine or abdomen/pelvis at any point in the postoperative period.
Descriptive statistics were used to compare cohorts: frequencies, chi-squared analysis for categorical variables, and t-test for continuous variables.
A total of 408 rostral pedicle screws were implanted in 204 patients (Robot: 102; Navigation: 306). Overall, 13 (12.3%) rostral facet joint violations were observed in the robot cohort and 75 (24.5%) in the navigation cohort (p=.01). Specifically, fewer robotic violations were observed at the L2 (3.5% vs 32.1%, p=.003) and L3 levels (3.9% vs 18.1%, p=.08) compared to navigation. No difference was observed at L4 and L5. Bilateral violations are significantly reduced with robotic approaches (5.3% vs 14.4%, p=.03). Lastly, more facet joint violations were observed during open approaches (robot: 18.8%, navigation: 27.3%) than percutaneous approaches (robot: 11.6%, navigation: 7.1%) in both groups (p<.001). The rate of L4 facet violations was 18.8% in the robotic cohort and 27.3% in the navigation cohort. The rate of L5 facet violations was 31.3% in the robotic cohort and 29.2% in the navigation cohort.
The use of robotic assistance in lumbar pedicle screws significantly reduced the rate of rostral facet joint violations compared to navigation guidance at L2 and L3 levels, but not at L4 and L5, with facet violations approaching nearly one-third of the patients at L5 screws. Rostral facet violations can significantly affect adjacent segment degeneration and disease. Technical factors and trajectory issues likely play a role and addressing these components should minimize unintended facet violation and proximal adding on 7).
Discussion
Many studies on facet joint violation (FJV) rely on retrospective analyses, which inherently carry selection bias. For example, Nilssen et al. conducted a retrospective matched cohort study comparing robotic and CT navigation-assisted pedicle screw placement, but the matching criteria (age, sex, and construct length) do not fully control for confounding variables such as surgeon experience, degenerative changes, and individual anatomical variations.
Moreover, the variability in grading systems (Babu, Shah, Park) presents challenges in standardizing findings across different studies. While interobserver reliability metrics have been reported (e.g., kappa coefficients ranging from 0.692 to 0.849), the clinical significance of these discrepancies remains underexplored.
The generalizability of findings is limited by sample sizes and study populations. Many studies focus on single-center experiences, which may not be representative of broader patient demographics or surgical practices. For instance, robotic-assisted studies often originate from high-resource centers with access to advanced technology, raising concerns about reproducibility in lower-resource settings.
a. Adjacent Segment Disease (ASD)
FJV has been implicated in accelerating adjacent segment degeneration (ASD), yet long-term follow-up data remain sparse. While retrospective analyses indicate a higher incidence of ASD in patients with facet violations, few studies extend beyond a two-year follow-up period. This is particularly concerning given that degenerative changes often manifest over longer timeframes.
Studies reporting increased revision surgery rates for ASD fail to isolate whether these revisions are directly attributable to FJV or to preexisting degenerative pathology. Longitudinal cohort studies with standardized imaging follow-ups would be required to clarify causality.
b. Chronic Pain and Functional Outcomes
While some studies report worse Oswestry Disability Index (ODI) and Visual Analog Scale (VAS) scores in FJV patients, pain is multifactorial. Factors such as psychosocial stressors, muscle imbalances, and preoperative pain levels confound these outcomes. Few studies incorporate validated patient-reported outcome measures (PROMs) beyond generic disability indices.
Additionally, while facet arthritis acceleration is postulated as a consequence of FJV, studies quantifying this progression via imaging biomarkers (e.g., MRI cartilage degradation scores) are lacking.
Technological advancements such as CT navigation and robotic assistance have been praised for reducing FJV rates (e.g., robotic-guided screws show lower L2–L3 violation rates than navigation-assisted screws). However, these benefits are not uniform across spinal levels, with L4–L5 violations remaining substantial.
Additionally, cost-effectiveness analyses are rarely included in these discussions. The economic burden of robotic systems—often exceeding $1 million—raises concerns about accessibility, particularly in public healthcare systems. While improved accuracy is documented, the absolute reduction in revision rates and long-term cost savings remain speculative.
Emerging techniques integrating artificial intelligence (AI) and augmented reality (AR) for surgical planning and intraoperative guidance show promise. However, existing literature predominantly consists of feasibility studies rather than robust randomized controlled trials (RCTs). Furthermore, AI models trained on historical datasets may perpetuate biases inherent in earlier techniques, necessitating continuous refinement and validation.
Future Directions and Recommendations
Future studies should prioritize prospective designs with longer follow-ups, ideally spanning 5–10 years, to capture delayed degenerative effects. Multicenter collaborations would enhance generalizability and mitigate single-institution biases.
The adoption of uniform grading systems, coupled with objective imaging assessments (e.g., MRI-based cartilage evaluation), would improve consistency across studies. Additionally, integrating PROMs tailored to spine pathology (e.g., SF-36, PROMIS measures) could provide a more comprehensive assessment of patient-reported outcomes.
While robotic and AI-assisted technologies demonstrate promise in reducing FJV rates, comprehensive cost-benefit analyses should accompany efficacy studies. These should consider not only equipment costs but also training, maintenance, and potential reductions in revision surgeries.
Conclusion
While technological advancements have improved pedicle screw accuracy and reduced facet joint violations, long-term evidence on clinical outcomes remains inconclusive. Future research must move beyond short-term radiographic assessments and emphasize functional outcomes, revision rates, and economic feasibility. Only through rigorous, standardized, and longitudinal studies can the true impact of FJV and its prevention strategies be fully understood.
While technological advances in spinal instrumentation have improved accuracy and reduced FJV rates, significant gaps remain in methodology, standardization, and long-term outcome assessment. Future research must move beyond short-term radiographic assessments and prioritize longitudinal, standardized, and economically viable studies to refine surgical decision-making and improve patient outcomes.