Table of Contents
Cervical Spine Radiography
Cervical Spine Radiography will fail to demonstrate canal narrowing due to thickening or inbuckling of ligamentum flavum, hypertrophy of facet joints, and poorly calcified spurs.
MRI: discloses compromise of the anterior spinal canal by discs or osteophytes (when combined with plain C-spine X-rays or CT, it increases the ability to differentiate osteophyte from traumatic disc herniation). Also good for evaluating ligamentum flavum.
Contour lines
On a lateral C-spine x-ray, there are 4 contour lines (AKA arcuate lines). Normally each should form a smooth, gentle curve
1. posterior marginal line (PML): along posterior cortical surfaces of vertebral bodies (VB). Marks the anterior margin of the spinal canal
2. anterior marginal line (AML): along anterior cortical surfaces of VBs.
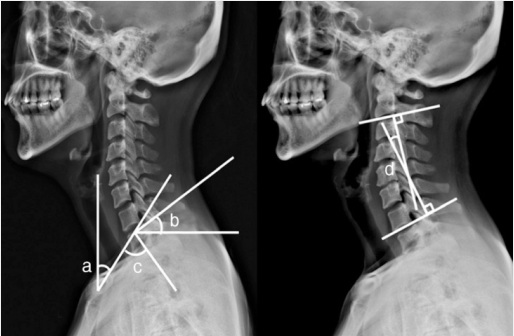
Schematic drawing of the measured angles of the cervicothoracic spine segments. a: Neck tilt; b: T1 slope; c: Thoracic inlet angle; d: C2 C7 angle.
Cervical lateral radiograph; b Detail of 36-inch lateral radiograph showing measurements a. Occiput-C2 sagittal Cobb angle, b. Occiput-C7 sagittal Cobb angle, c. C1-C2 sagittal Cobb angle, d. C2-C7 sagittal Cobb angle, e. T1 tilt. Horizontal solid white line: C1-C7 Sagittal Vertical Axis - distance between plumb line dropped from anterior tubercle of C1 and posterior superior corner of C7; Horizontal white dotted line: C2-C7 Sagittal Vertical Axis—distance between plumb line dropped from centroid of C2 and posterior superior corner of C7; White dashed line: Center of Gravity-C7 Sagittal Vertical Axis—distance between plumb line dropped from anterior margin of external auditory meatus and posterior superior corner of C7.
In pediatric traumatic brain injury, the use of cervical spine radiographs alone decreased between 2001 (47%) and 2011 (23%), with an annual decrease of 2.2% (95% confidence interval [CI], 1.1%-3.3%), and was largely replaced by an increased use of CT, with or without radiographs (8.6% in 2001 and 19.5% in 2011, with an annual increase of 0.9%; 95% CI, 0.1%-1.8%). A total of 2545 children received cervical spine CT despite being discharged alive from the hospital in less than 72 hours, and 1655 of those had a low-risk mechanism of injury.
The adoption of CT clearance of the cervical spine in adults seems to have influenced the care of children with traumatic brain injury TBI, despite concerns about radiation exposure 1).
The cervical spine series is a set of radiographs taken to investigate the bony structures of the cervical spine, albeit commonly replaced by the CT, the cervical spine series is an essential trauma radiograph for all radiographers to understand.
Indications
Cervical spine radiographs are indicated for a variety of settings including
trauma
infection
atypical pain
limb pain
osteoporosis
degenerative changes
A decision to pursue C-spine imaging of any kind should be cross-referenced with the 'Canadian C-Spine Rule' for C-spine imaging due to its high sensitivity and specificity
Projections
Standard projections
In the absence of CT views of the C-spine should be performed: AP, lateral, obliques and odontoid.
AP
anteroposterior projection of the cervical spine demonstrating the vertebral bodies and intervertebral spaces lateral often utilized in trauma demonstrated zygapophyseal joints soft tissue structures around the c spine spinous processes anterior-posterior relationship of the vertebral bodies odontoid also known as a 'peg' projection it demonstrates the C1 (atlas) and C2 (axis)
AP oblique
demonstrates the intervertebral foramina of the side positioned further from the image receptor
PA oblique
demonstrated the intervertebral foramina of the side positioned closer to the image receptor
Additional projections
cervicothoracic view (swimmer's view)
modified lateral projection of the cervical spine to visualize the C7/T1 junction
flexion-extension lateral
specialized projections of the cervical spine often requested to assess for spinal stability.
Fuchs view
non-angled AP radiograph of C1 and C2. It should not be used in a trauma setting
Cervical sagittal alignment
Body posture for Cervical Spine Radiography
Cervical Spine Magnetic Resonance Imaging
Cervical spine CT
Case series
2016
Seventy-four cases of 1-level anterior cervical discectomy and fusion (ACDF1) and 2-level ACDF (ACDF2) (40 ACDF1 and 34 ACDF2 procedures) were retrospectively reviewed. Upright neutral lateral cervical spine radiographs were assessed preoperatively and at 6 weeks and 1 year postoperatively. The measured radiographic parameters included focal lordosis, disc height, C2-7 lordosis, C1-7 lordosis, T1 slope, and C2-7 sagittal vertical axis. Correlation coefficients were calculated to determine the relationships between these radiographic measurements.
The mean values were as follows: preoperative focal lordosis was 0.574°, disc height was 4.48 mm, C2-7 lordosis was 9.66°, C1-7 lordosis was 42.5°, cervical sagittal vertebral axis (SVA) was 26.9 mm, and the T-1 slope was 33.2°. Cervical segmental lordosis significantly increased by 6.31° at 6 weeks and 6.45° at 1 year. C2-7 lordosis significantly improved by 1 year with a mean improvement of 3.46°. There was a significant positive correlation between the improvement in segmental lordosis and overall cervical lordosis. Overall cervical lordosis was significantly negatively correlated with cervical SVA. Improved segmental lordosis was not correlated with cervical SVA in ACDF1 patients but was significantly negatively correlated in ACDF2 patients. There was also a significant positive correlation between the T1 slope and cervical SVA.
In the study population, the improvement of focal lordosis was significantly correlated with an improvement in overall lordosis (C1-7 and C2-7), and overall lordosis as measured by the C2-7 Cobb angle was significantly negatively correlated with cervical SVA. Using lordotic cervical allografts, Gillis et al., successfully created and maintained significant improvement in cervical segmental lordosis at the 6-week and 1-year time points with values of 6.31° and 6.45°, respectively. ACDF is able to achieve statistically significant improvement in C2-7 cervical lordosis by the 1-year followup, with a mean improvement of 3.46°. Increasing the number of levels operated on resulted in improved cervical sagittal parameters. This establishes a baseline for further examination into the ability of multilevel ACDF to achieve cervical deformity correction through the intervertebral correction of cervical lordosis 2).