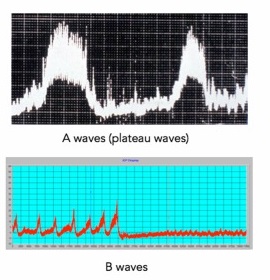
B-wave
In the context of intracranial pressure monitoring, a B wave refers to a specific pattern of ICP waveforms. B waves are slow, rhythmic oscillations of ICP that can be observed on a monitoring system. These waves may indicate fluctuations in intracranial pressure and can be associated with conditions like hydrocephalus or other neurological issues.
B-waves are more subtle than A-waves and can indicate several abnormalities of intracranial homeostasis including being an indicator of failing intracranial compensation. It is important to note however that they can also be present in patients with normal ICP. B waves are rhythmic oscillations with ICP rising in a crescendo manner to levels 20–30 mmHg higher than baseline, with a subsequent sharp decline. They occur every 1–2 min. Note, Lundberg A waves and B waves refer to raises in static (mean ICP) and are not related to the pressure fluctuations during the cardiac cycle, which is the case for ICP wave amplitudes
Repetitive transient intracranial pressure waveform elevations up to 50 mmHg (ICP B-waves) are often used to define pathological conditions and determine indications for ICP-reducing treatment.
Riedel et al. showed that nocturnal transient ICP elevations are present in patients without structural brain lesions or hydrocephalus in whom they are associated with sleep apnea. However, whether this signifies a general association between ICP macropatterns and sleep apnea remains unknown.
They included 34 patients with hydrocephalus, or idiopathic intracranial hypertension (IIH), who were referred to the Neurosurgical Department, Copenhagen, Denmark, from 2017 to 2021. Every patient underwent diagnostic overnight ICP monitoring for clinical indications, with simultaneous polysomnography (PSG) sleep studies. All transient ICP elevations were objectively quantified in all patients. Three patients were monitored with continuous positive airway pressure (CPAP) treatment for an additional night.
All patients had transient ICP elevations associated with sleep apnea. The mean temporal delay from sleep apnea to transient ICP elevations for all patients was 3.6 s (SEM 0.2 s). Ramp-type transient ICP elevations with a large increase in ICP were associated with rapid eye movement (REM) sleep and sinusoidal-type elevations with non-REM (NREM) sleep. In three patients treated with CPAP, the treatment reduced the number of transient ICP elevations with a mean of 37%. CPAP treatment resulted in insignificant changes in the average ICP in two patients but elevated the average ICP during sleep in one patient by 5.6 mmHg.
The findings suggest that sleep apnea causes a significant proportion of transient ICP elevations, such as B-waves, and sleep apnea should be considered in ICP evaluation. Treatment of sleep apnea with CPAP can reduce the occurrence of transient ICP elevations. More research is needed on the impact of slow oscillating mechanisms on transient ICP elevations during high ICP and REM sleep. 1)