Artificial neural network analysis
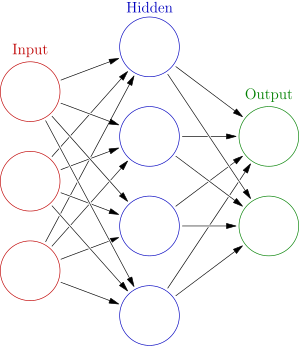
Artificial neural networks are generally presented as systems of interconnected “neurons” which exchange messages between each other. The connections have numeric weights that can be tuned based on experience, making neural nets adaptive to inputs and capable of learning.
For example, a neural network for handwriting recognition is defined by a set of input neurons which may be activated by the pixels of an input image. After being weighted and transformed by a function (determined by the network's designer), the activations of these neurons are then passed on to other neurons. This process is repeated until finally, the output neuron that determines which character was read is activated.
Like other machine learning methods – systems that learn from data – neural networks have been used to solve a wide variety of tasks, like computer vision and speech recognition, that are hard to solve using ordinary rule-based programming.
In machine learning and cognitive science, artificial artificial neural networks (ANNs) are a family of models inspired by biological neural networks (the central nervous systems of animals, in particular the brain) which are used to estimate or approximate functions that can depend on a large number of inputs and are generally unknown.
Using demographics and injury characteristics, as well as patient laboratory data, predictive tools (e.g., logistic regression [LR], support vector machine [SVM], decision tree [DT], naive Bayes [NB], and artificial neural networks [ANN]) were used to determine the mortality of individual patients. The predictive performance was evaluated by accuracy, sensitivity, and specificity, as well as by area under the curve (AUC) measures of receiver operator characteristic curves. In the training set, all five ML models had a specificity of more than 90% and all ML models (except the NB) achieved an accuracy of more than 90%. Among them, the ANN had the highest sensitivity (80.59%) in mortality prediction. Regarding performance, the ANN had the highest AUC (0.968), followed by the LR (0.942), SVM (0.935), NB (0.908), and DT (0.872). In the test set, the ANN had the highest sensitivity (84.38%) in mortality prediction, followed by the SVM (65.63%), LR (59.38%), NB (59.38%), and DT (43.75%).
The ANN model provided the best prediction of mortality for patients with isolated moderate and severe TBI 1).
An artificial neural network (ANN) was trained to classify 60 CSFPPWs in four different classes, according to their morphology, and its efficacy was compared to an expert examiner's classification. The morphology of CSFPPW, recorded in 60 patients at baseline, was compared to EI and Rout calculated at the end of an intraventricular infusion test to validate the utility of the proposed classification in patients' clinical evaluation.
The overall concordance in CSFPPW classification between the expert examiner and the ANN was 88.3 %. An elevation of EI was statistically related to morphological class' progression. All patients showing pathological baseline CSFPPW (class IV) revealed an alteration of CSF hydrodynamics at the end of their infusion test.
The proposed morphological classification estimates the global ICP wave and its ability to reflect or predict an alteration in CSF hydrodynamics. An ANN can be trained to efficiently recognize four different CSF wave morphologies. This classification seems helpful and accurate for diagnostic use 2).
Intracranial pressure (ICP) is commonly used by neurosurgeons as a source of valuable information about the current condition of the neurosurgical patient. Nevertheless, despite years of effort, extracting clinically valuable information from the ICP signal is still problematical. Approaches, using current values of ICP, may fail to disclose imminent risk, because unpredictable factors can rapidly change the properties of the signal. An alternative approach is to determine some global characteristics of the signal within a longer time interval and such statistical analyses have been proposed by several authors. A further, rarely considered, problem is assessment of the results obtained from the point of view of their practical utility and/or such classification of the obtained properties of the signal that they correspond to certain clinical states of the patient. While this might be a typical task for discriminant analysis, we approached the analysis using an alternative methodology, that of computational intelligence, implemented in artificial neural networks (ANN). We tested two variants of the ANN algorithms for classification and discrimination of global properties of the ICP signal. In a “dynamic pattern classification” the network was presented with several sections of ICP records together with information from the expert-neurosurgeon, classifying 4 risk groups. In this mode no data pre-processing was carried out, in contrast to our second approach, in which the signal had been pre-processed using published statistical analyses and only these intermediate coefficients were fed into the ANN classifier. The results obtained with both classification methods at their current stage of training were similar and approximated to a 70% rate of judgements consistent with the expert scoring. Nevertheless, the method based on the assessment of global parameters from the ICP record looks more promising, because it leaves the possibility for modification of the set of parameters analysed. The new parameters may include information extracted not only from the ICP signal, but also from other diagnostic modalities, like colour coded Doppler ultrasonography. The ultimate goal of this work is to build up a pseudo-intelligent computer expert system, which would be able to reason from a reduced set of input information, available from a standard monitoring modality, because it had been taught salient links between these data and higher-order data, upon which expert scoring was based 3).
artificial neural networks (ANN) were used to analyze the accuracy of outcome prediction after traumatic brain injury (TBI) for different combinations of clinical data and parameters derived from neuromonitoring. The total group included 95 patients suffering from TBI. For all patients clinical data (age, GCS, pupillary response etc.) were recorded and outcome was classified using Glasgow outcome scale after 6 months. In a first step a subgroup of 60 patients was chosen to train a neural network to predict outcome based only on clinical data. In a second step the resting 35 patients all having continuous neuromonitoring with automatic data storage of ICP and PtiO2 were chosen. Different network models were composed using the former clinical model plus up to three additional input units for the following parameters: (a) relative number of ICP > 40 mmHg, (b) relative number of PtiO2 < 5 mmHg and © relative number of ICP > 30 mmHg with simultaneous PtiO2 < 10 mmHg. For each model the following time periods were analyzed: day 1-2, day 1-3 and day 1-4 after trauma and additionally day 1-4 after trauma plus last day of neuromonitoring. Pure clinical data allowed to predict outcome with 74.3% accuracy. A combination of clinical data with ICP (a) significantly increased the confidence levels of outcome prediction in all time periods (p < 0.05) with accuracy rates rising up to 82.9% for the longer time periods. The combination of clinical data and ICP & PtiO2 © lead to comparable results. In contrast, no significant increases were observed in the early time periods when combining clinical data with PtiO2 (b) while accuracy rates rose up to 80% for extended time periods after trauma. A combination of all parameters lead to results lying between the above results. The results indicate that prediction of outcome can be improved by combining clinical and neuromonitoring data. The prognostic value of ICP might be superior to that of PtiO2 4).
Arle et al. applied neural network techniques to 80 consecutive patients undergoing epilepsy surgery in whom data on demographic, seizure, operative, and clinical variables to predict postoperative seizures were collected. Neural networks could be used to predict postoperative seizures in up to 98% of cases. Student's t-tests or chi-square analysis performed on individual variables revealed that only the preoperative medication index was significantly different (p = 0.02) between the two outcome groups. Six different combinations of input variables were used to train the networks. Neural network accuracies differed in their ability to predict seizures: using all data (96%); all data minus electroencephalography concordance and operative side (93%); all data except intra- or postoperative variables such as tissue pathological category (98%); all data excluding pathological category, intelligence quotient (IQ) data, and Wada results (84%); only demographics and tissue pathological category (65%); and only IQ data (63%).
Analysis of the results reveals that several networks that are trained with the usual accepted variables characterizing the typical evaluation of epilepsy patients can predict postoperative seizures with greater than 95% accuracy 5).
Artificial neural networks are used increasingly in applications such as graphic pattern recognition, which are difficult to address with conventional statistical methods. In the management of chronic pain, graphic methods are used routinely; patients describe their patterns of pain using “pain drawings.” The authors have previously reported an automated, computerized pain drawing methodology, which has been used by patients with implanted spinal cord stimulators to represent a technical goal of the procedure, the overlap of pain by stimulation paresthesias. Standard linear discriminant statistical methods have shown associations between stimulation parameters and electrode positions as independent variables and technical outcome and relief of pain as dependent variables. The authors have applied artificial neural networks to the problem of optimizing implanted stimulator adjustment. A data set of 3000 electrode combinations obtained in 41 patients was used to develop a linear discriminant statistical model on a mainframe computer and to train artificial neural networks on a personal computer. The performance of these two systems on a new data set obtained in 10 patients was compared with that of human “experts.” The best neural network model was marginally better than the linear discriminant model; the variance in patient ratings was predicted by these models to a degree that the human experts were unable to predict. The authors anticipate expanding the role of these models and incorporating them into expert systems for clinical use 6).
Azimi P, Mohammadi HR. Predicting endoscopic third ventriculostomy success in childhood hydrocephalus: an artificial neural network analysis. J Neurosurg Pediatr. 2014 Apr;13(4):426-32. doi: 10.3171/2013.12.PEDS13423. Epub 2014 Jan 31. PubMed PMID: 24483256.