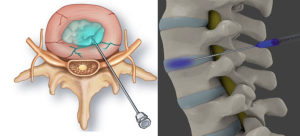
In a prospective real-world comparative study Sara Bisshopp et al. from Dr. Negrín University Hospital, Las Palmas published in the Journal of Clinical Medicine to compare clinical outcomes, hospital stay, and direct costs between initial intradiscal ozone treatment and standard microdiscectomy/discectomy in patients with lumbar disc herniation over a 24-month follow-up. Both groups experienced significant improvements in pain and disability scores. The ozone group had similar clinical outcomes to surgery but with significantly fewer surgical interventions (47% vs. 100%), shorter hospital stays, and reduced costs at 12 months 1).
Critical Appraisal
This study taps into a timely and pragmatic clinical question: Can minimally invasive ozone therapy reduce the surgical burden and costs while maintaining efficacy for lumbar disc herniation? While the 24-month prospective design and real-world context strengthen external validity, several methodological shortcomings temper enthusiasm.
First, the non-randomized design introduces considerable selection bias. The criteria for choosing ozone therapy vs. surgery, though labeled as “offered,” are not rigorously controlled. This self-selection can strongly influence outcomes. Second, sample size is modest (n=70), particularly when divided into two groups (32 ozone, 38 surgery), limiting statistical power.