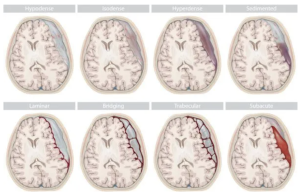
In a multicenter retrospective cohort study, Callen et al. — from the University of Colorado Anschutz, Kaiser Permanente Santa Clara, University of Freiburg, Cambridge University Hospitals, Newcastle upon Tyne Hospitals, Guy’s & St Thomas’s / King’s College Hospitals, and King’s College London — published in the American Journal of Neuroradiology, the clinical and radiologic outcomes of CT-guided epidural patching in patients with lateral dural tear causing spontaneous intracranial hypotension (SIH). The study also aimed to determine whether anatomic factors (e.g., herniated arachnoid pouch) or procedural variables (e.g., patch volume, material, approach) predict treatment success.
CT-guided patching led to complete symptom resolution in approximately one-third of patients. The presence of a herniated arachnoid pouch was associated with lower radiologic resolution of CSF collections. Procedural variables — such as patch type, approach, and volume — were not associated with outcomes. Notably, some patients experienced clinical improvement despite persistent CSF collections, highlighting the need for long-term follow-up and cautious reliance on imaging alone.