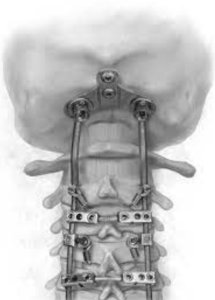
In a retrospective cohort study De Salvatore et al. from the Bambino Gesù Children’s Hospital, Rome; Università Campus Bio‑Medico di Roma, Rome published in the *Spine Deformity Journal* to assess radiographic correction and complications after final posterior spinal fusion in Early-Onset Scoliosis (EOS) patients initially treated with magnetically controlled growing rods (MCGR). Definitive fusion yields significant improvements in coronal curve (mean reduction from 45.5° to 33.5°) and thoracic kyphosis (from 19.8° to 13.5°), sustained at ≥2‑year follow‑up. Major complication rate was low (18.5%, one major) 1).
Critical review
– Strengths:
-
Focus on a clinically relevant patient group (walking EOS post-MCGR).
-
Objective measurement of both coronal and sagittal parameters with adequate follow-up.
– Limitations:
-
Small sample (n=27) limits statistical power and heterogeneity evaluation.