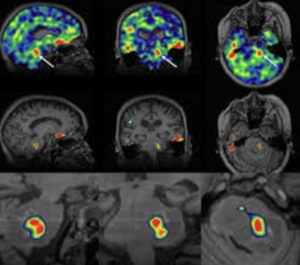
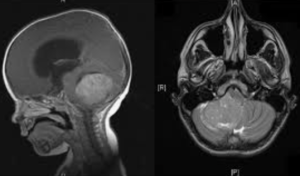
In a retrospective institutional experience with illustrative cases Shields LB et al. from the Norton Neuroscience Institute, Louisville published in Epilepsia Open to evaluate the role of the Surgical Theater (ST) 3D visualization system in enhancing presurgical planning for pediatric epilepsy surgery. The ST system enabled integration of multimodal imaging into immersive 3D models, improving collaborative surgical planning, enhancing intraoperative navigation, and allowing VR-based procedural rehearsal. It demonstrated utility across 85 cases and is posited as a promising adjunct for pediatric epilepsy surgical workflows 1)
Critical Review
This is a descriptive, non-comparative experience report centered on implementing the Surgical Theater (ST) system in a pediatric epilepsy context. While the authors present a visually compelling and potentially transformative workflow for presurgical planning, the study is methodologically weak—it lacks controls, quantifiable outcomes, or statistical rigor. The “results” are largely anecdotal, with 4 case examples insufficiently discussed in terms of surgical impact or clinical outcomes.