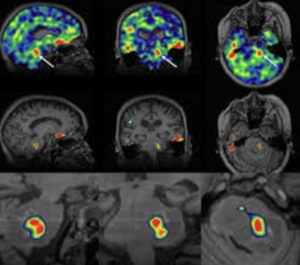
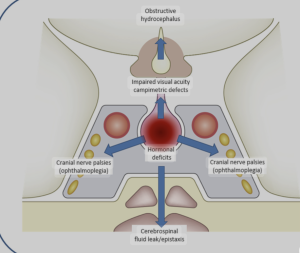
In a narrative review Bhatia et al. from the Children’s Hospital of Philadelphia, Radiological Sciences Laboratory, School of Medicine, Stanford University, published in the American Journal of Neuroradiology to explore the potential of sodium-23 MRI (^23Na-MRI) as a noninvasive imaging modality to assess physiological and biochemical changes in pediatric brain tumors and concluded that is a promising, noninvasive imaging modality capable of providing unique physiological and biochemical information that is not accessible through conventional MRI techniques
This narrative review attempts to position ^23Na-MRI as a frontier imaging technique for pediatric brain tumors. It lauds the modality’s potential to reveal sodium-dependent physiological alterations — but quickly devolves into technological evangelism with minimal clinical anchoring. The piece is high on optimism, low on pragmatism, and entirely devoid of data-supported clinical outcomes.
🧠 1. Conceptual Inflation: “Promise” Without Proof
The article enthusiastically describes the theoretical virtues of sodium MRI — sensitivity to cell integrity, ionic gradients, extracellular space — but offers no compelling clinical cases, no comparative metrics, and no outcome data. What remains is a speculative wish list, presented as a roadmap. The authors confuse imaging potential with diagnostic utility, a common pitfall in radiology reviews driven by physics rather than patient care.
“Exciting” is not a scientific category.