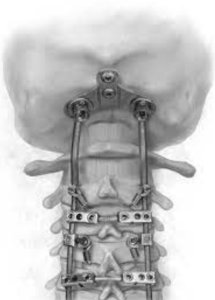
In a retrospective cohort study Shahin et al. from the Doernbecher Children’s Hospital and Oregon Health & Science University, Portland published in the Journal of Neurosurgery Pediatrics to assess whether screw‑fixed autologous rib grafts improve fusion rates in pediatric occipitocervical fusion (OCF), and validate a novel imaging-based fusion grading scale independent of graft type. Screw‑anchored rib autograft achieved 100 % solid fusion at ≥3 months (n=16), compared to 57 % fusion (4/7) and 43 % resorption/pseudarthrosis in standard allograft/BMP group (p=0.0066). The new 0–2 radiographic grade correlated well with CT-defined outcomes 11)
Critical review
1. Study design & cohort: Retrospective, single‑institution, relatively small sample (n=21 total; final rib‑graft cohort n=17 minus one without CT). Comparison spans two eras (2015–2016 vs. 2016–2022), risks secular trends or surgeon learning‑curve bias.
2. Intervention vs. control: Cohort 1 received standard instrumentation with allograft/BMP; cohort 2 received screw‑fixed rib graft. But several cohort 2 cases were revisions from cohort 1, confounding the groups. No randomization.
3. Outcomes & follow-up: Fusion assessed at ≥3 months by blinded neuroradiologists with a 0–2 grading scale—clear and reproducible. However, mid / long‑term (>1 year) follow-up beyond early fusion rate not well characterized.
4. Results interpretation: Dramatic fusion improvement is compelling, but may reflect both graft technique and instrumentation changes over time. Lack of halo/BMP/lab comparisons limiting.
5. Radiographic grading scale: Solid concept, but needs external validation across graft types and institutions.
6. Safety & complications: No donor‑site morbidity or hardware failures reported over 5+ years. But small sample limits detection of rare complications.
7. Limitations:
Small size, retrospective design, era bias, limited demographic detail (syndromic vs. non‑syndromic outcomes), no clinical outcome measures (e.g. neurological, hardware-related pain).
8. Generalisability: Promising technique; should be validated via prospective multicentre trials with longer follow‑up and clinical metrics.
Final verdict: 7/10
Takeaway for practicing neurosurgeons:
Pediatric OCF augmented with screw‑fixed rib autograft appears to reliably achieve solid arthrodesis by 3 months without added donor‑site morbidity. Consideration of this technique is warranted, especially in revision cases or patients at high nonunion risk. Adopting the novel radiographic grading scale may standardize fusion reporting across centres.
Bottom line:
Screw-anchored rib autograft in pediatric OCF offers markedly improved short‑term fusion rates (100 % vs. 43 %) with minimal morbidity. Yet prospective data and long‑term outcomes are needed before widespread adoption.
Category: Pediatric Neurosurgery, Spine Surgery Tags: occipitocervical fusion, rib autograft, pediatric, spinal arthrodesis, radiographic grading, fusion rate