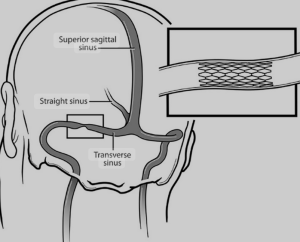
In a retrospective, multi-institutional, multinational propensity score-matched database analysis Jarunee Intrapiromkul et al. from the WVU Rockefeller Neuroscience Institute, Morgantown published in the Journal of NeuroInterventional Surgery with the purpose to compare the efficacy and healthcare impact of Transverse sinus stenting versus cerebrospinal fluid shunting in patients with idiopathic intracranial hypertension (IIH) using a large-scale health data platform. TVS stenting was associated with significantly lower treatment failure, fewer residual symptoms (except pulsatile tinnitus), and reduced healthcare utilization at 1 year, suggesting superiority over CSF shunting in these metrics 7).
Scientific Rigor and Methodology: The use of the TriNetX database provides substantial sample size and multi-institutional representation. However, as a retrospective design, this study inherits the usual limitations—selection bias, reliance on accurate diagnostic and procedural coding, and the inability to adjust for all clinical confounders (e.g., anatomical variants, patient preference, and local practice patterns). Propensity score matching does help mitigate these concerns but does not fully equate to randomized trial robustness.
Notably, the study defines treatment failure using repeat intervention rates, a proxy that may miss functional deterioration or subtle visual decline not resulting in reoperation. The lack of granular ophthalmologic outcome data (e.g., perimetry, OCT, visual acuity) and longitudinal follow-up beyond one year are conspicuous absences. Moreover, symptom-based outcomes like “headache” and “visual disturbances” are inherently subjective and inconsistently documented in administrative datasets, potentially undermining reliability.
Tone and Structure: The article is clearly written and appropriately structured for a high-impact neurosurgical journal, maintaining a neutral and data-driven tone. The abstract effectively conveys primary findings, though it leans toward promotional language when describing “promising” results without emphasizing limitations.
Accuracy and Clinical Utility: While the data compellingly favor stenting in terms of re-intervention and readmission rates, this paper does little to stratify patient populations or offer practical selection criteria. Clinically relevant nuance—such as stenosis severity, pressure gradient thresholds, or anatomical predictors of shunt failure—is entirely absent. For practicing neurosurgeons, especially those evaluating IIH management strategies, the study provides surface-level guidance but fails to inform surgical decision-making in detail.
The increased odds of persistent pulsatile tinnitus post-stenting is acknowledged but not explored, leaving a potentially critical caveat underdeveloped.
Unaddressed Weaknesses: – No breakdown of procedural complications (e.g., stent thrombosis, infection, shunt malfunction) – No visual outcome metrics or neuro-ophthalmologic validation – Lacks subgroup analysis by demographic or comorbid profiles – Entirely dependent on coding integrity within TriNetX – One-year horizon may underestimate late shunt failures
Overall Verdict
Takeaway for Neurosurgeons: This study supports a shift toward TVS stenting in appropriate IIH patients, primarily due to reduced need for subsequent procedures and lower healthcare burden. However, selection criteria remain vague, and the clinical decision should still be individualized based on anatomy, vision status, and local expertise.
Bottom Line: TVS stenting appears superior to CSF shunting in terms of repeat intervention rates and healthcare utilization, but methodological limitations and lack of detailed clinical granularity curb its practice-changing value.
Rating: 6.5/10
Corresponding Author Email: dhairyalakhani@gmail.com
Intrapiromkul J, Rai AT, Lakhani DA. Transverse venous sinus stenting versus cerebrospinal fluid shunting in idiopathic intracranial hypertension: a multi-institutional and multinational database study. J Neurointerv Surg. 2025 Jun 27:jnis-2025-023699. doi: 10.1136/jnis-2025-023699. Epub ahead of print. PMID: 40579154.