In a retrospective cohort study Sioutas et al. from the Virginia Commonwealth University Health System, Richmond published in JAMA Neurology to evaluate whether GLP-1 receptor agonist (GLP-1 RA) therapy is associated with improved outcomes in patients with idiopathic intracranial hypertension (IIH), compared to conventional therapies.
Conclusions: In a large matched cohort drawn from a nationwide EHR database (TriNetX), GLP-1 RA therapy was significantly associated with lower medication burden, reduced symptoms (headache, papilledema, visual disturbances), fewer surgical interventions, and lower 1-year mortality. These benefits were not paralleled by significant differences in BMI, suggesting mechanisms beyond weight loss. Bariatric surgery yielded more weight loss but inferior clinical outcomes compared to GLP-1 RA use. The study suggests a promising role for GLP-1 RAs in IIH management, though causality remains unproven 1).
Summary of Findings
GLP-1 RAs were associated with:
↓ Medication burden
↓ Symptoms: headache, papilledema, visual disturbance
↓ Surgical interventions
↓ 1-year mortality
No significant difference in BMI change
Bariatric surgery achieved greater weight loss but inferior clinical outcomes
Authors’ Conclusion: GLP-1 RAs may provide benefit in IIH independent of weight loss, warranting further study.
Critical Review
1. Design Strengths:
Large nationwide dataset (TriNetX), increasing statistical power
Matching for baseline characteristics reduces—but does not eliminate—confounding
Clinically relevant composite endpoints
2. Methodological Caveats:
Retrospective EHR-based design is inherently limited by:
Missing or imprecise clinical detail (e.g. visual field data, CSF pressure)
Possible misclassification or underreporting of IIH diagnosis and outcomes
Mortality reduction is surprising and biologically implausible in the IIH context without clearer pathophysiological explanation or granular cause-of-death data
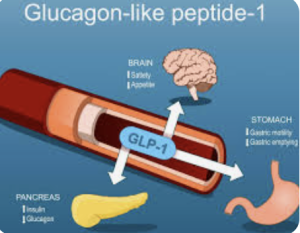
Lack of BMI change challenges the dominant theory that GLP-1 RAs benefit IIH primarily through weight reduction. This discrepancy raises the possibility of off-target or pleiotropic effects—or, more cautiously, of residual confounding or reverse causality
3. Interpretation Gaps:
The superior outcomes compared to bariatric surgery—despite lower weight loss—are counterintuitive and poorly explored
No analysis of adherence, dose-response, or specific GLP-1 RA agents (semaglutide vs liraglutide, etc.)
Lack of CSF dynamics data prevents insight into plausible mechanisms
4. Clinical Relevance:
The enthusiasm for GLP-1 RAs in neurology (migraines, neuroprotection, now IIH) is growing, but this study does not cross the threshold for clinical adoption
A significant risk of overinterpretation exists due to striking outcomes derived from non-randomized data
Final Appraisal
Verdict: Cautiously promising, but far from practice-changing. The reduction in interventions and mortality is intriguing but may reflect database artifacts or unmeasured confounders more than therapeutic efficacy.
Takeaway for Neurosurgeons: GLP-1 RAs might become part of the future non-surgical armamentarium in IIH, but do not justify altering current surgical thresholds or indications.
Bottom Line: A hypothesis-generating study. Prospective, ideally randomized trials are needed to determine if GLP-1 RAs truly offer disease-modifying benefits in IIH—or if this is statistical noise dressed as progress.
Score: 6.5/10 (Robust analysis, provocative results, but weak mechanistic support and unproven causality)