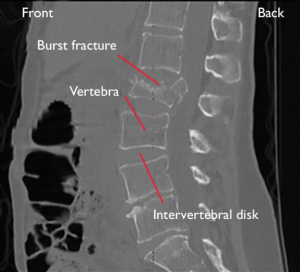
In a Prospective multicentre cohort study Dvorak et al. from the University of British Columbia ( – Vancouver), Univ. Medical Center Utrecht, Malteser Waldrankenhaus St. Marien (Erlangen), Univ. of Washington (Seattle), etc. published in the Global Spine Journal to examine whether surgical vs non‑surgical treatment accelerates clinically meaningful improvement (MCID of 12.8 points ODI) in neurologically intact thoracolumbar burst fracture patients within 1 year. Similar median time to reach MCID in both groups (~25 days). Post‑hoc suggests surgery may achieve ‘minimal disability’ (ODI <20) faster (69 vs 82 days; P=0.057). Larger trials needed 2)
Critical Appraisal
-
Strengths: Prospective design, multicentre/international inclusion enhances generalizability; uses accepted ODI threshold.
-
Limitations: Not randomized—treatment selection bias possible; statistical power limited—non-significant trend (P=0.057) may be false negative; outcome centered on ODI improvement, lacking radiographic, complication, or cost analysis within this paper.
-
Contextual relevance: Prior literature shows conservative/surgical outcomes similarly effective in absence of neuro deficit but differing in other domains. Earlier RCTs and meta‑analyses support equivalence
-
Gaps: Absence of blinding, heterogeneity in surgical technique, missing cost‑utility analysis and long‑term outcome data; Posterior Ligamentous Complex Integrity subgroup underpowered.
Verdict (0–10)
6/10 – Well‑executed prospective cohort, but limited by non-random allocation, underpowered to detect meaningful secondary outcomes, and lacking comprehensive endpoints.
Takeaway for Practice
Non‑operative management remains a valid first-line option in neurologically intact TL burst fractures for reducing disability. Surgery might offer earlier return to near-normal function in select patients but requires further evidence. Decisions should be individualized based on imaging (Posterior Ligamentous Complex Integrity), patient preference, comorbidity, and resource availability.
Bottom Line
In neurologically intact thoracolumbar burst fractures, surgical intervention does not hasten achievement of the Oswestry Disability Index – Minimal Clinically Important Difference (ODI MCID) but may modestly accelerate return to minimaldisability. Without randomized evidence or cost-benefit data, non-operative management remains a reasonable default; surgical timing should prioritize patient selection and shared decision-making.
Dvorak MF, Öner CF, Dandurand C, Schnake KJ, Bransford RJ, Popescu EC, El-Sharkawi M, Rajasekaran S, Benneker LM, Schroeder GD, Tee JW, France JC, Paquet J, Allen R, Lavelle WF, Hirschfeld M, Pneumaticos S, Vialle E, Vaccaro AR. Surgical versus Non-Surgical Treatment of Thoracolumbar Burst Fractures in Neurologically Intact Patients: A Prospective International Multicentre Cohort Study. Global Spine J. 2025 Jul 3:21925682251356910. doi: 10.1177/21925682251356910. Epub ahead of print. PMID: 40605521.