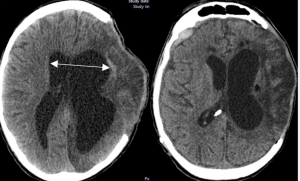
In a retrospective observational cohort study Romualdo et al. from the Department of Neurosurgery Faculty of Medicine, Technische Universität Dresden University Hospital Carl Gustav Carus published in the Neurosurgical Review to identify clinical, radiological, and surgical risk factors associated with the development of shunt-dependent posttraumatic hydrocephalus (PTH) in patients who underwent decompressive craniectomy following severe traumatic brain injury (TBI). Shunt-dependent post-traumatic hydrocephalus (PTH) occurred in 27% of patients after decompressive craniectomy for severe TBI. Independent risk factors included older age, basal cistern subarachnoid hemorrhage, post-traumatic ischemic infarcts, transcalvarial herniation, subdural hygroma, and progressive contusion hemorrhages. Surgical parameters were not predictive. Patients requiring shunt placement had significantly worse neurological outcomes 5).
🚨 The Illusion of Multidimensionality Despite claiming a “multidimensional” analysis, the study delivers a monotonous list of obvious associations—many of which have been reported in the literature for over a decade. Subarachnoid hemorrhage, infarction, hygroma, contusion progression… yes, thank you, we knew that. What’s new? Almost nothing.
📉 Retrospective, Predictable, and Predictively Useless While the authors apply multivariate statistics, no predictive model or clinical score is produced. The result? A study that identifies risk factors after the shunt has already been placed — a textbook example of retrospective confirmation bias without translational benefit.
🩺 Surgical Variables: Studied but Ignored The study promises to explore surgical factors, but then dismisses them as statistically insignificant without deeper analysis. Was it the timing? The size of the craniectomy? The bone flap location? None of these variables are interrogated meaningfully. A missed opportunity to challenge surgical dogmas.
⚖️ Outcome Data: Obvious and Overstated Shunted patients had worse outcomes? Of course they did. But without adjusting for injury severity, comorbidities, or ICU complications, the conclusion becomes medically tautological — not enlightening.
🧠 Neurological Subtlety? Nowhere to Be Found No cognitive testing. No neuropsychological follow-up. No differentiation between communicating vs. non-communicating hydrocephalus. The brain is treated like a binary sponge: swollen or drained.
🧪 Innovation Score: 2/10
✅ Decent sample size
✅ Inclusion of volumetric imaging
❌ No dynamic monitoring
❌ No external validation
❌ No actionable tools for clinicians
❌ No change in practice likely
💬 Final Verdict
“A technically competent autopsy of well-known correlations, marketed as innovation. This is not multidimensional analysis — it’s dimensional padding.”
Unless you’re building a PowerPoint on PTH incidence for a basic residency lecture, this paper offers no clinical leverage, no predictive advantage, and no intellectual disruption. Neurosurgeons looking for guidance will leave empty-handed — again.
Romualdo SMF, Juratli TA, Eyüpoglu I, Schackert G, Dengl M, Prem M, Hijazi MM, Sitoci-Ficici KH. Post-traumatic hydrocephalus after decompressive craniectomy: a multidimensional analysis of clinical, radiological, and surgical risk factors. Neurosurg Rev. 2025 Jun 21;48(1):523. doi: 10.1007/s10143-025-03673-0. PMID: 40542880